 A woman suffers a heart attack every 90 seconds in the United States. Yet according to a 2009 American Heart Association survey only half of women indicated they would call 9-1-1 if they thought they were having a heart attack and few were aware of the most common heart attack symptoms.
A woman suffers a heart attack every 90 seconds in the United States. Yet according to a 2009 American Heart Association survey only half of women indicated they would call 9-1-1 if they thought they were having a heart attack and few were aware of the most common heart attack symptoms.
The Make the Call. Don't Miss a Beat. campaign is a national public education campaign that aims to educate, engage, and empower women and their families to learn the seven most common symptoms of a heart attack and encourage them to call 9-1-1 as soon as those symptoms arise.
The first step toward surviving a heart attack is learning to recognize the symptoms. The campaign, developed by the U.S. Department of Health and Human Services' Office on Women's Health, encourages woman to make the call to 9-1-1 immediately if they experience one or more of the heart attack symptoms listed below. The most common signs of heart attack in both women and men are:
Unusually heavy pressure on the chest, like there's a ton of weight on you
Most heart attacks involve chest pain or discomfort in the center or left side of the chest. It usually lasts for more than a few minutes or goes away and comes back. It can feel like uncomfortable pressure, squeezing, fullness, or pain. It may even feel like heartburn or indigestion.
Sharp upper body pain in the neck, back, and jaw
This symptom can include pain or discomfort in one or both arms, the back, shoulders, neck, jaw, or upper part of stomach (not below the belly button). Pain in the back, neck, or jaw is a more common heart attack symptom for women than it is for men.
Severe shortness of breath
This symptom can come on suddenly. It may occur while you are at rest or with minimal physical activity. You may struggle to breathe or try taking deep breaths. Shortness of breath may start before or at the same time as chest pain or discomfort, and can even be your only symptom.
Cold sweats, and you know it's not menopause
Unexplained or excessive sweating, or breaking out into a "cold sweat," can be a sign of heart attack.
Unusual or unexplained fatigue (tiredness)
Sudden and unusual tiredness or lack of energy is one of the most common symptoms of heart attack in women, and one of the easiest to ignore. It can come on suddenly or be present for days. More than half of women having a heart attack experience muscle tiredness or weakness that is not related to exercise.
Unfamiliar dizziness or light-headedness
Unlike in the movies, most heart attacks do not make you pass out right away. Instead, you may suddenly feel dizzy or light-headed.
Unexplained nausea (feeling sick to the stomach) or vomiting
Women are twice as likely as men to experience nausea, vomiting, or indigestion during their heart attack. These feelings are often written off as having a less serious cause. Remember, nausea and vomiting may be signs that something is seriously wrong, especially if you have other symptoms.
If you have any one of these symptoms and it lasts for more than five minutes, call 9-1-1 for emergency medical care. Even if your symptoms go away in less than five minutes, call your doctor right away—it could be a sign that a heart attack is coming soon. Don't waste time trying home remedies or waiting for the feelings to pass on their own. Remember, quick treatment can save your life.

 Women with peripheral artery disease (PAD) lose ability to walk short distances and climb stairs sooner than men.
Women with peripheral artery disease (PAD) lose ability to walk short distances and climb stairs sooner than men. In celebration of Women's Heart Month, the Institute for Women's Health Research featured heart disease in women in its February E-newsletter. To view this free newsletter, click
In celebration of Women's Heart Month, the Institute for Women's Health Research featured heart disease in women in its February E-newsletter. To view this free newsletter, click  Women who report having high job strain have a 40 percent increased risk of cardiovascular disease, including heart attacks and the need for procedures to open blocked arteries, compared to those with low job strain, according to research presented at the American Heart Association's Scientific Sessions 2010.
Women who report having high job strain have a 40 percent increased risk of cardiovascular disease, including heart attacks and the need for procedures to open blocked arteries, compared to those with low job strain, according to research presented at the American Heart Association's Scientific Sessions 2010. Two scientific articles in the July 2010 issue of American Journal of Clinical Nutrition shed more insight on the chemistry of red wine that may explain why more doctors are suggesting that a little red wine may be heart-healthy. Both articles focus on resveratrol, a chemical compound found in certain plants. It is called a phytoalexin because plants naturally produce it as an antibiotic substance to fight both bacteria and fungi. Plants containing resveratrol include the grapes and skins of grapes that produce wine, raspberries, mulberries, blueberries and cranberries. There is growing evidence that resveratrol plays a role in plaque development, fatty tissue growth, and other biological mechanisms that impact the cardiovascular system.
Two scientific articles in the July 2010 issue of American Journal of Clinical Nutrition shed more insight on the chemistry of red wine that may explain why more doctors are suggesting that a little red wine may be heart-healthy. Both articles focus on resveratrol, a chemical compound found in certain plants. It is called a phytoalexin because plants naturally produce it as an antibiotic substance to fight both bacteria and fungi. Plants containing resveratrol include the grapes and skins of grapes that produce wine, raspberries, mulberries, blueberries and cranberries. There is growing evidence that resveratrol plays a role in plaque development, fatty tissue growth, and other biological mechanisms that impact the cardiovascular system.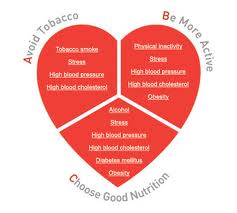 CHICAGO --- Is cardiovascular health in middle age and beyond a gift from your genes or is it earned by a healthy lifestyle and within your control?Two large studies from Northwestern Medicine confirm a healthy lifestyle has the biggest impact on cardiovascular health. One study shows the majority of people who adopted healthy lifestyle behaviors in young adulthood maintained a low cardiovascular risk profile in middle age. The five most important healthy behaviors are not smoking, low or no alcohol intake, weight control, physical activity and a healthy diet. The other study shows cardiovascular health is due primarily to lifestyle factors and healthy behavior, not heredity.
CHICAGO --- Is cardiovascular health in middle age and beyond a gift from your genes or is it earned by a healthy lifestyle and within your control?Two large studies from Northwestern Medicine confirm a healthy lifestyle has the biggest impact on cardiovascular health. One study shows the majority of people who adopted healthy lifestyle behaviors in young adulthood maintained a low cardiovascular risk profile in middle age. The five most important healthy behaviors are not smoking, low or no alcohol intake, weight control, physical activity and a healthy diet. The other study shows cardiovascular health is due primarily to lifestyle factors and healthy behavior, not heredity.
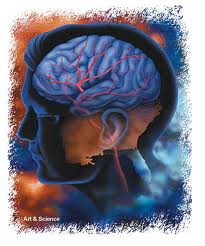 Between 2000 and 2007, the death rate of men treated in hospitals for stroke tumbled by 29 percent compared to a 24 percent decline for women, according to the latest News and Numbers from the Agency for Healthcare Research and Quality (AHRQ).
Between 2000 and 2007, the death rate of men treated in hospitals for stroke tumbled by 29 percent compared to a 24 percent decline for women, according to the latest News and Numbers from the Agency for Healthcare Research and Quality (AHRQ).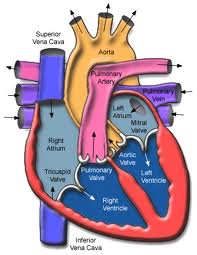
 Aspirin therapy to prevent heart attack may have different benefits and harms in men and women.
Aspirin therapy to prevent heart attack may have different benefits and harms in men and women. U.S. Preventive Services Task Force, Ann Intern Med 150(6):396-404, 2009 (AHRQ supports the Task Force). See also Optowsky, McWilliams, and Cannon, J Gen Intern Med 22:55-61, 2007 (AHRQ grant T32 HS00020).
U.S. Preventive Services Task Force, Ann Intern Med 150(6):396-404, 2009 (AHRQ supports the Task Force). See also Optowsky, McWilliams, and Cannon, J Gen Intern Med 22:55-61, 2007 (AHRQ grant T32 HS00020).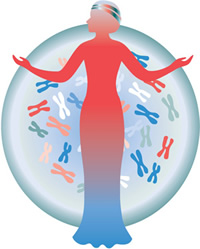 The National Institutes of Health Office of Research on Women's Health (ORWH) will celebrate its 20th anniversary with a day-long symposium on Monday, Sept. 27, in Bethesda, Maryland. Discussed will be highlights of early accomplishments in women's health research, as well as a preview of the next decade A Vision for the Year 2020. Many of the advances involve medical differences between women and men, and implications for sex/gender — appropriate clinical care and personalized medicine.
The National Institutes of Health Office of Research on Women's Health (ORWH) will celebrate its 20th anniversary with a day-long symposium on Monday, Sept. 27, in Bethesda, Maryland. Discussed will be highlights of early accomplishments in women's health research, as well as a preview of the next decade A Vision for the Year 2020. Many of the advances involve medical differences between women and men, and implications for sex/gender — appropriate clinical care and personalized medicine.