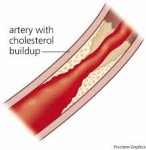
 Early results of the ELITE study find women who started hormone therapy early after menopause saw a significant slowing of atherosclerotic progression, whereas those who waited more than a decade saw no impact on vascular health, supporting the "timing hypothesis".
Early results of the ELITE study find women who started hormone therapy early after menopause saw a significant slowing of atherosclerotic progression, whereas those who waited more than a decade saw no impact on vascular health, supporting the "timing hypothesis".
"ELITE results are consistent with the majority of the literature that shows that women who are young and/or in close proximity to menopause when starting hormone therapy have reduced coronary heart disease and overall mortality," according to study leader Howard N. Hodis, MD, of the University of Southern California in Los Angeles, and colleagues.
The Women's Health Initiative, aiming for cardiovascular prevention with menopausal hormone therapy, had raised major concerns about stroke and myocardial infarction (MI) in its somewhat older, later menopause population. The KEEPS study subsequently showed that for a younger (ages 42 to 58) population, this may not be true.
ELITE was designed to directly test the hypothesis that timing makes all the difference in safety of hormone therapy after menopause.
"I think it's important that clinicians not interpret this as you should start estrogen to try to prevent heart disease, but that the younger, newly menopausal woman who has menopausal symptoms should not be denied hormone therapy because of concerns about heart disease risk, as was seen in older women," JoAnn E. Manson, MD, of Brigham and Women's Hospital in Boston, told MedPage Today.
"There are other factors to take into consideration [such as risk of thrombosis]," she explained. "But because a newly menopausal woman is generally at low absolute risk of heart attack, stroke, thrombosis, all of those outcomes, it tends to be a favorable balance of benefit-to-risk."
While suggestive that early hormone therapy wouldn't have an impact on later heart disease risk, "this trial wasn't large enough to look at clinical events," Manson cautioned.
To learn more about this study, click HERE. To learn more about Menopause, click HERE.
Primary source: American Heart Association
Source reference: Hodis HN, et al "Testing the menopausal hormone therapy timing hypothesis: The early versus late intervention trial with estradiol" AHA 2014; Abstract 13283.

 Drinking milk is not just for kids but also for post-menopausal women, new research shows. A new study from the Women's Health Initiative just published by the North American Menopause Society, reveals that calcium and vitamin D after menopause can improve women's cholesterol profiles.
Drinking milk is not just for kids but also for post-menopausal women, new research shows. A new study from the Women's Health Initiative just published by the North American Menopause Society, reveals that calcium and vitamin D after menopause can improve women's cholesterol profiles. The next time you see your primary care doctor, he or she will have access to updated guidelines and a new electronic tool that can better predict your chances of developing cardiovascular disease, including heart attack and stroke.
The next time you see your primary care doctor, he or she will have access to updated guidelines and a new electronic tool that can better predict your chances of developing cardiovascular disease, including heart attack and stroke. Young and middle-age women whose diet included high levels of anthocyanins -- the flavonoids present in red and blue fruits such as strawberries and blueberries -- had a significantly reduced risk for myocardial infarction (MI), a large prospective study found.
Young and middle-age women whose diet included high levels of anthocyanins -- the flavonoids present in red and blue fruits such as strawberries and blueberries -- had a significantly reduced risk for myocardial infarction (MI), a large prospective study found. For years we criticized heart researchers for not including women in the early studies that recommended aspirin to prevent heart disease. We asked: How can you recommend aspirin in women when all the studies took place in males! In 2007, after additional studies that included females, the American Heart Association released guidelines for the CVD preventive care in women including aspirin. Their recommendations:
For years we criticized heart researchers for not including women in the early studies that recommended aspirin to prevent heart disease. We asked: How can you recommend aspirin in women when all the studies took place in males! In 2007, after additional studies that included females, the American Heart Association released guidelines for the CVD preventive care in women including aspirin. Their recommendations: Consuming a low carbohydrate-high protein diet -- like the Atkins diet -- may be associated with a greater risk of cardiovascular disease in women. Decreases in carbohydrate intake and increases in protein intake were all associated with significantly greater risks of incident cardiovascular disease events in young Swedish women, according to Pagona Lagiou, MD, PhD, of the University of Athens in Greece, and colleagues.
Consuming a low carbohydrate-high protein diet -- like the Atkins diet -- may be associated with a greater risk of cardiovascular disease in women. Decreases in carbohydrate intake and increases in protein intake were all associated with significantly greater risks of incident cardiovascular disease events in young Swedish women, according to Pagona Lagiou, MD, PhD, of the University of Athens in Greece, and colleagues. Heart disease and stroke deaths drop significantly for people with diabetes!
Heart disease and stroke deaths drop significantly for people with diabetes! Ireland, a land of "happy wars and sad love songs," is also a nation that is adopting some of the bad eating habits found in the U.S. and is trying to break those habits.
Ireland, a land of "happy wars and sad love songs," is also a nation that is adopting some of the bad eating habits found in the U.S. and is trying to break those habits. Heart disease is the leading cause of death among women, and evidence-based national guidelines promote the use of daily aspirin for women at increased risk for cardiovascular disease. However, less than half of the women who could benefit from aspirin are taking it, according to an article available free online at the
Heart disease is the leading cause of death among women, and evidence-based national guidelines promote the use of daily aspirin for women at increased risk for cardiovascular disease. However, less than half of the women who could benefit from aspirin are taking it, according to an article available free online at the