 Do you have questions about menopause? Are you ever curious about hormone therapy treatments? You’re not alone! Every year over two million women in America alone enter into menopause, and most have questions. The Women’s Health Research Institute wants to provide answers with our informational menopause website: menopause.northwestern.edu. This site is tailored to the needs of women, offering up-to-date information on menopause and symptom management. The site even offers a personalized “Menopause Self Assessment,” which enables women to evaluate their own symptoms and health status that they can then print out and share with their healthcare providers.
Do you have questions about menopause? Are you ever curious about hormone therapy treatments? You’re not alone! Every year over two million women in America alone enter into menopause, and most have questions. The Women’s Health Research Institute wants to provide answers with our informational menopause website: menopause.northwestern.edu. This site is tailored to the needs of women, offering up-to-date information on menopause and symptom management. The site even offers a personalized “Menopause Self Assessment,” which enables women to evaluate their own symptoms and health status that they can then print out and share with their healthcare providers.
Menopause marks the transition in every woman’s life when menstruation and fertility decline and eventually end. Menopause symptoms affect women differently, so treatments vary from woman to woman. The many stages of menopause may seem overwhelming, but women should find comfort in the numerous treatment options developed by leading researchers and clinicians. Empowering women with educated choices regarding their health provides them with the tools to live longer and stronger in their journey during and after menopause. Click here to learn more about menopause and the different ways you can navigate your menopausal transition.

 Back in the early 2000s flawed reports surfaced that suggested hormone replacement therapy (HRT) was linked to increased risks of heart disease and breast, ovarian and womb cancers--scientists recently concluded these theories are false. This new research, which followed women for a decade, has found no evidence that HRT is linked to any life-threatening condition! This is good news for the millions of menopausal women who may want to use HRT to control their hot flashes, night sweats, and depression.
Back in the early 2000s flawed reports surfaced that suggested hormone replacement therapy (HRT) was linked to increased risks of heart disease and breast, ovarian and womb cancers--scientists recently concluded these theories are false. This new research, which followed women for a decade, has found no evidence that HRT is linked to any life-threatening condition! This is good news for the millions of menopausal women who may want to use HRT to control their hot flashes, night sweats, and depression. Vasomotor symptoms, mainly in the form of hot flashes, are the most commonly reported menopausal symptom. While many people assumed a connection, data was inconsistant, it was only recently that cross sectional survey using the Menopause Health Questionnaire from Mayo Clinic was conducted that compared users and non-users of caffeine beverages. A total of 2,507 surveys were completed and after adjusting for menopause status and smoking (caffeine users smoked more than non-users), the researchers found that caffeine users reportied higher vasomotor symptom scores.
Vasomotor symptoms, mainly in the form of hot flashes, are the most commonly reported menopausal symptom. While many people assumed a connection, data was inconsistant, it was only recently that cross sectional survey using the Menopause Health Questionnaire from Mayo Clinic was conducted that compared users and non-users of caffeine beverages. A total of 2,507 surveys were completed and after adjusting for menopause status and smoking (caffeine users smoked more than non-users), the researchers found that caffeine users reportied higher vasomotor symptom scores. 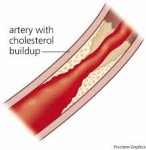 Early results of the ELITE study find women who started hormone therapy early after menopause saw a significant slowing of atherosclerotic progression, whereas those who waited more than a decade saw no impact on vascular health, supporting the "timing hypothesis".
Early results of the ELITE study find women who started hormone therapy early after menopause saw a significant slowing of atherosclerotic progression, whereas those who waited more than a decade saw no impact on vascular health, supporting the "timing hypothesis". Today, Many women live beyond age 80 and as a result may be postmenopausal for over 30 years. Each woman has a unique range of symptoms. Hormone therapy has been widely prescribed since the early 60s despite limited research to relieve unpleasant menopausal symptoms. However, alarms were raised in the 1990's that have led to a whole battery of new research on hormone therapy that continues to this day.
Today, Many women live beyond age 80 and as a result may be postmenopausal for over 30 years. Each woman has a unique range of symptoms. Hormone therapy has been widely prescribed since the early 60s despite limited research to relieve unpleasant menopausal symptoms. However, alarms were raised in the 1990's that have led to a whole battery of new research on hormone therapy that continues to this day. Perimenopause is the time when a women naturally starts having menopausal symptoms. This natural change usually lasts about a year and is often referred to as the 'menopause transition'. At this time, fertility declines but a woman may still get pregnant, and effective birth control should be used if she does not want to have a mid-life baby. Generally, after a year of no menses, a woman can be considered infertile and menopausal.
Perimenopause is the time when a women naturally starts having menopausal symptoms. This natural change usually lasts about a year and is often referred to as the 'menopause transition'. At this time, fertility declines but a woman may still get pregnant, and effective birth control should be used if she does not want to have a mid-life baby. Generally, after a year of no menses, a woman can be considered infertile and menopausal. As more post menopausal women change to a low dose local vaginal estrogen to control vaginal atrophy, a group of experts have recommended that the FDA modify the package Black Box Warning label on the product packaging. The current warning is based on research done mainly on
As more post menopausal women change to a low dose local vaginal estrogen to control vaginal atrophy, a group of experts have recommended that the FDA modify the package Black Box Warning label on the product packaging. The current warning is based on research done mainly on  The average age of menopause in the United States is around 51 years old, but the onset can widely vary. Premature menopause refers to menopause of onset at or before 40 years of age. This can occur because of a variety of causes, including surgery (i.e. bilateral oophorectomy, removal of ovaries), chemotherapy or pelvic radiation treatments for cancer, chromosomal or genetic defects, and spontaneous premature ovarian failure.
The average age of menopause in the United States is around 51 years old, but the onset can widely vary. Premature menopause refers to menopause of onset at or before 40 years of age. This can occur because of a variety of causes, including surgery (i.e. bilateral oophorectomy, removal of ovaries), chemotherapy or pelvic radiation treatments for cancer, chromosomal or genetic defects, and spontaneous premature ovarian failure. Most women think menopause means low estrogen, hot flashes, and the end to regular and monthly periods. This may not be the case, however. Researchers have found that women may experience an increase in the amount and duration of bleeding, which may occur sporadically throughout the transition of menopause.
Most women think menopause means low estrogen, hot flashes, and the end to regular and monthly periods. This may not be the case, however. Researchers have found that women may experience an increase in the amount and duration of bleeding, which may occur sporadically throughout the transition of menopause.