 Young women with the menopause-like condition, primary ovarian insufficiency, are much more likely than other women to experience depression at some point during their lives, according to a study from the National Institutes of Health. The finding suggests that all women diagnosed with the condition should be evaluated for depression.
Young women with the menopause-like condition, primary ovarian insufficiency, are much more likely than other women to experience depression at some point during their lives, according to a study from the National Institutes of Health. The finding suggests that all women diagnosed with the condition should be evaluated for depression.
Depression is a serious medical illness affecting the brain which involves more than feeling blue or sad for a few days. Symptoms include persistent feelings of sadness, difficulty sleeping or over sleeping, energy loss, and feelings of worthlessness.
Primary ovarian insufficiency, or POI, results in a menopause-like condition years before normal menopause begins — sometimes as early as the teens or twenties. Women with POI stop producing normal amounts of reproductive hormones, develop hot flashes, and typically become infertile. The study authors evaluated 174 women with POI and found that 67 percent either were currently clinically depressed or had been depressed at least one time in their lives.
The researchers noted that this proportion was more than twice the rate of depression found by a national survey of women in the general population.
"Because of the strong association with depression, our results indicate all women diagnosed with POI should be thoroughly evaluated for depression," said Lawrence M. Nelson, M.D., co-senior author of the study and head of the Integrative and Reproductive Medicine Group at the NIH’s Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD). "Simply asking patients if they are depressed is not sufficient. Primary care physicians should evaluate their patients with a diagnostic screening test to determine if treatment or referral to a mental health specialist for further evaluation is needed."
The study's first author was Peter J. Schmidt, M.D., of the National Institute of Mental Health (NIMH). The study appears in The Journal of Clinical Endocrinology and Metabolism.
The study was unable to determine why women with POI are more likely than other women to experience depression. The investigators cited results of a previous study, which had suggested that depression might trigger physical changes that ultimately lead women to develop POI. However, in the current study, more than 73 percent of women with POI first experienced depressive symptoms after developing the irregular menstrual cycles believed to be an indicator of impending POI.
The findings also did not support the hypothesis that most women with POI become depressed after they are told of their diagnosis, when they learn that they will likely be infertile. In the current study, more than 68 percent of patients with POI who had depression had become depressed after the onset of irregular menstrual cycles, but before receiving the diagnosis of POI.
In a previous study, Dr. Schmidt found that women entering natural menopause at an appropriate age are at greater risk of depression late in the menopause transition, when estrogen levels are particularly low.
"Future studies are needed to help determine whether hormonal changes, perhaps combined with a particular genetic makeup, might predispose some women to depression," said Dr. Schmidt.
The authors also noted that studies of women undergoing natural menopause have found that estrogen supplements relieve symptoms of depression in some women. The authors added that it is possible that estrogen supplements might relieve symptoms of depression in women with POI.
NIMH provides information about women and depression in its booklet Women and Depression: Discovering Hope.


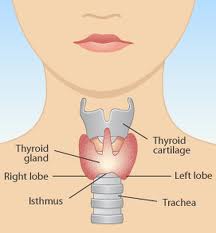 The American Cancer Society projects the U.S. incidence of thyroid cancer in 2010 at 44,670 cases (14.4 cases per 100,000 people) with women having 3 times the rate of men. The rate of thyroid cancer diagnosis has doubled since 1990, in large part because of improved diagnosis, but also because of unknown factors.
The American Cancer Society projects the U.S. incidence of thyroid cancer in 2010 at 44,670 cases (14.4 cases per 100,000 people) with women having 3 times the rate of men. The rate of thyroid cancer diagnosis has doubled since 1990, in large part because of improved diagnosis, but also because of unknown factors.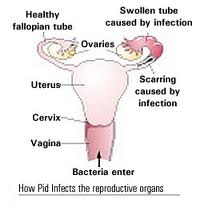 Pelvic inflammatory disease (PID) refers to infection of the uterus (womb), fallopian tubes and other reproductive organs that causes symptoms such as lower abdominal pain. It is a serious complication of some sexually transmitted diseases, especially chlamydia and gonorrhea. PID can damage the fallopian tubes and tissues in and near the uterus and ovaries and can lead to serious consequences including infertility, ectopic pregnancy (a pregnancy in the fallopian tube or elsewhere outside the womb), abscess formation and chronic pelvic pain.
Pelvic inflammatory disease (PID) refers to infection of the uterus (womb), fallopian tubes and other reproductive organs that causes symptoms such as lower abdominal pain. It is a serious complication of some sexually transmitted diseases, especially chlamydia and gonorrhea. PID can damage the fallopian tubes and tissues in and near the uterus and ovaries and can lead to serious consequences including infertility, ectopic pregnancy (a pregnancy in the fallopian tube or elsewhere outside the womb), abscess formation and chronic pelvic pain. December 1 is World AIDS Day and the
December 1 is World AIDS Day and the  Two scientific articles in the July 2010 issue of American Journal of Clinical Nutrition shed more insight on the chemistry of red wine that may explain why more doctors are suggesting that a little red wine may be heart-healthy. Both articles focus on resveratrol, a chemical compound found in certain plants. It is called a phytoalexin because plants naturally produce it as an antibiotic substance to fight both bacteria and fungi. Plants containing resveratrol include the grapes and skins of grapes that produce wine, raspberries, mulberries, blueberries and cranberries. There is growing evidence that resveratrol plays a role in plaque development, fatty tissue growth, and other biological mechanisms that impact the cardiovascular system.
Two scientific articles in the July 2010 issue of American Journal of Clinical Nutrition shed more insight on the chemistry of red wine that may explain why more doctors are suggesting that a little red wine may be heart-healthy. Both articles focus on resveratrol, a chemical compound found in certain plants. It is called a phytoalexin because plants naturally produce it as an antibiotic substance to fight both bacteria and fungi. Plants containing resveratrol include the grapes and skins of grapes that produce wine, raspberries, mulberries, blueberries and cranberries. There is growing evidence that resveratrol plays a role in plaque development, fatty tissue growth, and other biological mechanisms that impact the cardiovascular system. CHICAGO --- Estrogen is an elixir for the brain, sharpening mental performance in humans and animals and showing promise as a treatment for disorders of the brain such as Alzheimer’s disease and schizophrenia. But long-term estrogen therapy, once prescribed routinely for menopausal women, now is quite controversial because of research showing it increases the risk of cancer, heart disease and stroke.Northwestern Medicine researchers have discovered how to reap the benefits of estrogen without the risk. Using a special compound, they flipped a switch that mimics the effect of estrogen on cortical brain cells. The scientists also found how estrogen physically works in brain cells to boost mental performance, which had not been known.
CHICAGO --- Estrogen is an elixir for the brain, sharpening mental performance in humans and animals and showing promise as a treatment for disorders of the brain such as Alzheimer’s disease and schizophrenia. But long-term estrogen therapy, once prescribed routinely for menopausal women, now is quite controversial because of research showing it increases the risk of cancer, heart disease and stroke.Northwestern Medicine researchers have discovered how to reap the benefits of estrogen without the risk. Using a special compound, they flipped a switch that mimics the effect of estrogen on cortical brain cells. The scientists also found how estrogen physically works in brain cells to boost mental performance, which had not been known.
 In a new meta-analysis published in the
In a new meta-analysis published in the  November is the busiest month of the year for the US Department of Agriculture Meat & Poultry Hotline. During the week of Thanksgiving(November 25), they get lots of questions about how to safely cook a turkey. Here are answers to some of the more common questions.
November is the busiest month of the year for the US Department of Agriculture Meat & Poultry Hotline. During the week of Thanksgiving(November 25), they get lots of questions about how to safely cook a turkey. Here are answers to some of the more common questions.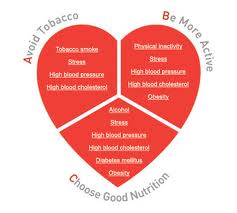 CHICAGO --- Is cardiovascular health in middle age and beyond a gift from your genes or is it earned by a healthy lifestyle and within your control?Two large studies from Northwestern Medicine confirm a healthy lifestyle has the biggest impact on cardiovascular health. One study shows the majority of people who adopted healthy lifestyle behaviors in young adulthood maintained a low cardiovascular risk profile in middle age. The five most important healthy behaviors are not smoking, low or no alcohol intake, weight control, physical activity and a healthy diet. The other study shows cardiovascular health is due primarily to lifestyle factors and healthy behavior, not heredity.
CHICAGO --- Is cardiovascular health in middle age and beyond a gift from your genes or is it earned by a healthy lifestyle and within your control?Two large studies from Northwestern Medicine confirm a healthy lifestyle has the biggest impact on cardiovascular health. One study shows the majority of people who adopted healthy lifestyle behaviors in young adulthood maintained a low cardiovascular risk profile in middle age. The five most important healthy behaviors are not smoking, low or no alcohol intake, weight control, physical activity and a healthy diet. The other study shows cardiovascular health is due primarily to lifestyle factors and healthy behavior, not heredity.