 For some unknown reason, we are suddenly receiving a lot of comments on our March 2010 posting on Endometriosis. Maybe it is because endometriosis is one of the most common gynecological diseases, affecting more that 5.5 million women in North America alone. There is a comprehensive fact sheet available from the National Institute of Child Health and Human Development on this topic that is very helpful. Click here to view the information.
For some unknown reason, we are suddenly receiving a lot of comments on our March 2010 posting on Endometriosis. Maybe it is because endometriosis is one of the most common gynecological diseases, affecting more that 5.5 million women in North America alone. There is a comprehensive fact sheet available from the National Institute of Child Health and Human Development on this topic that is very helpful. Click here to view the information.
 The millions of middle-aged and older adults who suffer from insomnia have a new drug-free prescription for a more restful night’s sleep. Regular aerobic exercise improves the quality of sleep, mood and vitality, according to a small but significant new study from Northwestern Medicine and the Feinberg School of Medicine. Insomnia is more prevalent in women.
The millions of middle-aged and older adults who suffer from insomnia have a new drug-free prescription for a more restful night’s sleep. Regular aerobic exercise improves the quality of sleep, mood and vitality, according to a small but significant new study from Northwestern Medicine and the Feinberg School of Medicine. Insomnia is more prevalent in women.
The study is the first to examine the effect of aerobic exercise on middle-aged and older adults with a diagnosis of insomnia. About 50 percent of people in these age groups complain of chronic insomnia symptoms. The aerobic exercise trial resulted in the most dramatic improvement in patients’ reported quality of sleep, including sleep duration, compared to any other non-pharmacological intervention.
“This is relevant to a huge portion of the population,” said Phyllis Zee, M.D., director of the Sleep Disorders Center at Northwestern Medicine and senior author of a paper to be published in the October issue of Sleep Medicine. The lead author is Kathryn Reid, research assistant professor at Feinberg.
“Insomnia increases with age,” Zee said. “Around middle age, sleep begins to change dramatically. It is essential that we identify behavioral ways to improve sleep. Now we have promising results showing aerobic exercise is a simple strategy to help people sleep better and feel more vigorous.” The drug-free strategy also is desirable, because it eliminates the potential of a sleeping medication interacting with other drugs a person may be taking, Reid said.
Sleep is an essential part of a healthy lifestyle, like nutrition and exercise, noted Zee, a professor of neurology, neurobiology, and physiology at Northwestern University Feinberg School of Medicine and a physician at Northwestern Memorial Hospital.
“Sleep is a barometer of health, like someone’s temperature. It should be the fifth vital sign. If a person says he or she isn’t sleeping well, we know they are more likely to be in poor health with problems managing their hypertension or diabetes," notes Zee.
The study included 23 sedentary adults, primarily women, 55 and older who had difficulty falling sleep and/or staying asleep and impaired daytime functioning. Women have the highest prevalence of insomnia. After a conditioning period, the aerobic physical activity group exercised for two 20-minute sessions four times per week or one 30-to-40-minute session four times per week, both for 16 weeks. Participants worked at 75 percent of their maximum heart rate on at least two activities including walking or using a stationary bicycle or treadmill.
Participants in the non-physical activity group participated in recreational or educational activities, such as a cooking class or a museum lecture, which met for about 45 minutes three to five times per week for 16 weeks. Both groups received education about good sleep hygiene, which includes sleeping in a cool, dark and quiet room, going to bed the same time every night and not staying in bed too long, if you can’t fall asleep.
Exercise improved the participants’ self-reported sleep quality, elevating them from a diagnosis of poor sleeper to good sleeper. They also reported fewer depressive symptoms, more vitality and less daytime sleepiness. “Better sleep gave them pep, that magical ingredient that makes you want to get up and get out into the world to do things,” Reid said.
The participants’ scores on the Pittsburgh Sleep Quality Index dropped an average of 4.8 points. (A higher score indicates worse sleep.) In a prior study using t’ai chi as a sleep intervention, for example, participants’ average scores dropped 1.8 points.
“Exercise is good for metabolism, weight management and cardiovascular health and now it’s good for sleep,” Zee said.
The research was funded by the National Institute on Aging.
Source: Marla Paul - health sciences editor at the NU Feinberg School of Medicine
 An understanding why women experience more stress-related mental disorders like depression and Post Traumatic Stress Disorder (PTSD) has eluded scientists but a new study in rat brains may help explain why women are more prone to mood and anxiety disorders than men.
An understanding why women experience more stress-related mental disorders like depression and Post Traumatic Stress Disorder (PTSD) has eluded scientists but a new study in rat brains may help explain why women are more prone to mood and anxiety disorders than men.
In order to better understand this study, I found it helpful to look up a few key definitions:
- stressor: a stimulus that causes stress, can be physical, emotional or social
- hormone: a secretion of an endocrine gland that is transmitted by the blood to the tissue on which it has an effect
- neurotransmitter: a chemical that transmits signals from a neuron (nerve system cell) to a cell across an empty space called a "synapse"
- receptor: a protein molecule embedded in either the membrane or cytoplasm of a cell, to which one or more specific kinds of signaling molecules, such as a neurotransmitter or hormone may attach. Each cell typically has many receptors, of many different kinds.
Now, back to the study:
Corticotropin releasing factor (CRF), which acts as both a hormone and a neurotransmitter, is likely a key player. In response to a stressor, CRF binds to receptors on cells in an alarm center deep in the brainstem, called the locus ceruleus. This telegraphs heightened emotional arousal throughout the brain via the chemical messenger norepinephrine. Such hyper-arousal can be adaptive for brief periods, but not if it becomes chronic. Runaway CRF is a core feature of depression.
Previous studies suggested that this alarm system is more sensitive to CRF and stress in the female brain and researchers at Children's Hospital in Philadelphia developed an experiment to see how CRF receptors responded in male versus female rats, both unstressed and after exposure to a stressor (in this case, a swim).
Even in the absence of any stress, the researchers found the female stress signaling system to be more sensitive from the start. CRF receptors had stronger connections or coupling in the female rats, so it took lower levels of CRF to activate proteins in the unstressed females compared to males. CRF levels that had no effect in males turned on cells in female rats.
After stress, CRF receptors remained exposed on the neuronal membranes in the female rat, maintaining the CRF effect. In the stressed male, the CRF receptors interacted with proteins in the cell that enabled some of the them to retreat and not be available to couple to the CRF. This helped the male brain adapt its sensitivity to the stressor and thus the stress response was less than in the females.
What is the significance of this experiment? Certain brain cells in females are more sensitive to CRF and less able to adapt to too much CRF than male brain cells.
The next step is to examine the male and female CRF receptors for structural differences that might account for the functional differences (e.g., response to stress, depression). Since most rodent models of mood and anxiety disorders use male animals exclusively, the new findings of sex differences in stress signaling mechanisms call for a more sex- and gender-balanced approach---especially for mental disorders that disproportionately affect females. This sex-difference should also be factored in as medication treatments based on blocking CRF receptor are developed, say the researchers.
Source: Sex differences in corticotropin-releasing factor receptor signaling and trafficking: potential role in female vulnerability to stress-related psychopathology. Mol Psychiatry. 2010 Jun 15. (PMID: 20548297)

Our monthly women's health e-newsletter is now available on the Institute for Women's Health Research web site. Learn more about smoking, women and lung cancer. You can also check out our website every month to get the lastest e-newsletter for free.
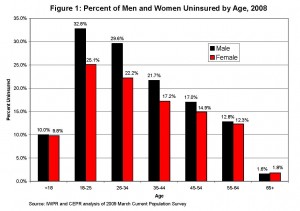
Contrary to some commonly held beliefs, men, more than women will likely benefit more from expanded healthcare coverage. According to the Institute for Women's Policy Research June 2010 Fact Sheet, men represent a majority of non-elderly US adults who lack health insurance across all age groups but particularly ages 18-34. Under age 18, boys and girls with health insurance have nearly the same coverage with many insured under public plans. The jump begins when students leave their parents' plan at either high school or college graduation. This will definitely improve when the Affordable Care Act of 2010 (ACA) becomes effective on September 23, 2010 and raises the age a young adult can stay on their parents' plans.
One of the reasons young women have better coverage is the fact that they have access to healthcare through Medicaid which has traditionally provided a safety net for family planning and pregnancy coverage for those with low or no income.
As we age, and reach 55 years and older, this difference is less between men and women. Medicare coverage that generally begins at age 65 is universal and fewer than 2 % of men or women lack health insurance once they reach this age group.
If you are interested in reading more about insurance differences between the sexes, visit the IWPR site
 The National Institutes of Health Office of Research on Women's Health (ORWH) will celebrate its 20th anniversary with a day-long symposium on Monday, Sept. 27, in Bethesda, Maryland. Discussed will be highlights of early accomplishments in women's health research, as well as a preview of the next decade A Vision for the Year 2020. Many of the advances involve medical differences between women and men, and implications for sex/gender — appropriate clinical care and personalized medicine.
The National Institutes of Health Office of Research on Women's Health (ORWH) will celebrate its 20th anniversary with a day-long symposium on Monday, Sept. 27, in Bethesda, Maryland. Discussed will be highlights of early accomplishments in women's health research, as well as a preview of the next decade A Vision for the Year 2020. Many of the advances involve medical differences between women and men, and implications for sex/gender — appropriate clinical care and personalized medicine.
A keynote speaker will be former NIH Director Bernadine Healy, M.D., who launched the Women's Health Initiative (WHI), a $625-million effort to study the causes, prevention, and cures of diseases that affect women at midlife and beyond. The WHI study continues to uncover critical information, including recent evidence that combined hormone replacement therapy carries a greater risk for heart attack and stroke than previously thought, particularly in older women.
The scientific keynoter will be Linda G. Griffith, Ph.D., professor and chair of MIT's Biological and Mechanical Engineering Department. She will discuss the integration of tissue engineering and systems biology in women's health research. A scheduled guest speaker in the afternoon is actress Cicely Tyson, who won three Emmy Awards and was nominated for an Academy Award for her portrayals of strong, positive African-American women. Her women's medical research interests include high blood pressure, heart disease and stroke, especially in minority patients. Her acting career, begun in 1957, remains active. This will be her first visit to the NIH campus.
The free and open symposium will conclude with a reception honoring many of the women and men who are heroes of women's health research. For more details, visit http://orwh.od.nih.gov or call ORWH at 301-402-1770.
 Weight gain during menopause continues to be a challenge to women. About 30% of women aged 50-59 are not just overweight, but obese. This weight gain increases one's risk for high blood pressure, heart disease, and diabetes. Just when we are getting used to the other symptoms often associated with menopause (hot flashes, insomnia, etc), we now have to worry about other serious chronic diseases! It's hard not to say, "aging is not for sissies".
Weight gain during menopause continues to be a challenge to women. About 30% of women aged 50-59 are not just overweight, but obese. This weight gain increases one's risk for high blood pressure, heart disease, and diabetes. Just when we are getting used to the other symptoms often associated with menopause (hot flashes, insomnia, etc), we now have to worry about other serious chronic diseases! It's hard not to say, "aging is not for sissies".
So why does menopause add those unwanted inches? Scientists and physicians indicate that it is probably due to a number of factors related to both menopause and aging.
In animal studies, estrogen appears to help regulate body weight. With lower estrogen levels, lab animals tend to eat more and be less physically active. Reduced estrogen may also lower metabolic rate (rate at which the body converts stored energy into working energy). It is possible that the same thing happens to women when their estrogen level drops at menopause. There is some evidence that estrogen hormone therapy may increase one's resting metabolic rate, slowing weight gain.
Other factors for this weight gain are related to aging. As we age, we exercise less. This leads to increased loss of muscle mass, which decreases our resting metabolism even more! This makes it easier to gain weight. As we age, our aerobic capacity also declines (the rate we use up energy during exercise). To compensate for this, we may need to increase the amount of time we exercise in order to achieve the same weight loss we experienced while exercising when when we were younger.
To learn more how exercise can help control menopausal weight gain and some tips for ensuring success, click here.
 Women with the most serious type of angina are three times as likely as men with the same condition to develop severe coronary artery disease (CAD), researchers have found.
Women with the most serious type of angina are three times as likely as men with the same condition to develop severe coronary artery disease (CAD), researchers have found.
In the study, Canadian researchers analyzed the medical records of 23,771 patients referred for a first diagnostic angiography. They found that women over age 60 with the most serious type of angina (Class IV) had a 21 percent higher absolute risk of developing CAD than did men. Women younger than 60 had an 11 percent greater risk of CAD than men in the same age group.
When the researchers factored in other variables commonly associated with CAD -- such as diabetes, high blood pressure, high cholesterol, smoking and age -- they found that Class IV angina increased the risk of CAD by 82 percent in women and 28 percent in men.
The study also found that men were more likely to have severe CAD than women (37 percent versus 22 percent) and that women with severe CAD tended to be significantly older than men with severe CAD (70 years versus 66 years).
The study findings are published in the July issue of the Journal of Internal Medicine.
"CAD is the leading cause of ill health and death in men and women in the western world, accounting for over a third of deaths. In fact, more women die from CAD than breast disease every year. Despite this, there is still a persistent perception that CAD is a man's disease," lead author Catherine Kreatsoulas, of the department of clinical epidemiology and biostatistics at McMaster University in Hamilton, Ontario, said in a news release from the journal's publisher.
However, the university's research found that women who have what the Canadian Cardiovascular Society defines as Class IV angina -- which means they are unable to perform any activity without symptoms and even suffer angina at rest -- "are significantly more likely to develop severe CAD than men with the same condition," Kreatsoulas added.
The findings are crucial for doctors deciding which patients should be referred for coronary angiography, Kreatsoulas said.
SOURCE: Journal of Internal Medicine, news release, July 8, 2010.
Copyright (c) 2010 HealthDay. All rights reserved.
 Our recent blog on male menopause has generated a number of questions, especially on the side effects of hormone treatments. I went back to Dr. Robert Brannigan, a Northwestern University urologist, who was quoted in our previous blog on the topic for guidance and he shared an article that was jointly prepared by the Practice Committee of the American Society for Reproductive Medicine and the Society for Male Reproduction and Urology entitled, "Androgen deficiency in the aging male" (Fertility and Sterility, Vol. 90, Suppl 3, November 2008). It should be noted that although there are recommendations (see below) for androgen replacement therapy for older men, the data to support treatment protocols are based on a limited number of clinical trials. Furthermore, the long term health risks and benefits of androgen therapy in the older man are not well defined so it is important that anyone undergoing androgen therapy be carefully monitored.
Our recent blog on male menopause has generated a number of questions, especially on the side effects of hormone treatments. I went back to Dr. Robert Brannigan, a Northwestern University urologist, who was quoted in our previous blog on the topic for guidance and he shared an article that was jointly prepared by the Practice Committee of the American Society for Reproductive Medicine and the Society for Male Reproduction and Urology entitled, "Androgen deficiency in the aging male" (Fertility and Sterility, Vol. 90, Suppl 3, November 2008). It should be noted that although there are recommendations (see below) for androgen replacement therapy for older men, the data to support treatment protocols are based on a limited number of clinical trials. Furthermore, the long term health risks and benefits of androgen therapy in the older man are not well defined so it is important that anyone undergoing androgen therapy be carefully monitored.
All commercial androgen formulation currently available in the US are preparations of testosterone, an androgen that can be converted to estradiol. The potential risks of androgen therapy in older men include fluid retention, gynecomastia, excessively elevated red blood cell mass, exacerbation of sleep apnea, benign or malignant prostate disease, and an increase in risk for cardiovascular disease (CVD).
The Summary and Recommendations of the report state:
- Androgen deficiency in the aging male may be associated with changes in mood, body composition, stamina, energy, and decreased sexual and cognitive function as well as loss of bone mineral density. Such signs and symptoms may be relieved or eliminated with testosterone replacement therapy.
- Serum testosterone should be evaluated only in men with signs or symptoms of androgen deficiency.
- Androgen therapy should be considered for men who have symptoms of androgen deficiency and a low serum total testosterone concentration (<200 ng/dL).
- Free or bioavailable testosterone levels or the free testosterone index should be evaluated in men who have symptoms of androgen deficiency and a borderline total serum testosterone concentration between 200 ng/dL and 400 ng/dL.
- During androgen therapy, serum testosterone, PSA (prostate specific antigen), and hematocrit (level of red blood cells) should be monitored, and periodic digital rectal exam is recommended.
- Limited data regarding the benefits and risks of testosterone replacement therapy do not permit specific treatment recommendations at this time and further research studies are needed to better define the effects of androgen replacement therapy in aging men.
Men considering androgen replacement therapy may want to consider participation in a clinical trial so that we can increase our knowledge in this area.
 A new study underscores the importance for women with a family history of breast or ovarian cancer to get genetic counseling and testing for the BRCA1 and BRCA2 genes that make them more likely to develop lethal breast or ovarian cancer, says a Northwestern Medicine oncologist. The study, which was published in the Sept. 1 issue of the Journal of the American Medical Association (JAMA), shows women with the gene live longer and nearly eliminate their risk of cancer by having prophylactic surgeries to remove their ovaries and fallopian tubes (salpingo-oophorectomy) or their breasts in a mastectomy.
A new study underscores the importance for women with a family history of breast or ovarian cancer to get genetic counseling and testing for the BRCA1 and BRCA2 genes that make them more likely to develop lethal breast or ovarian cancer, says a Northwestern Medicine oncologist. The study, which was published in the Sept. 1 issue of the Journal of the American Medical Association (JAMA), shows women with the gene live longer and nearly eliminate their risk of cancer by having prophylactic surgeries to remove their ovaries and fallopian tubes (salpingo-oophorectomy) or their breasts in a mastectomy.
“This is the first study to prove women survive longer with these preventive surgeries and shows the importance of genetic testing when there is a family history of early breast or ovarian cancer,” said Virginia Kaklamani, M.D., co-author of an accompanying editorial in JAMA. Kaklamani is director of translational breast cancer research at the Robert H. Lurie Comprehensive Cancer Center of Northwestern University. She also is an associate professor of medicine at Northwestern University Feinberg School of Medicine and an oncologist at Northwestern Memorial Hospital.
In the editorial, Kaklamani and coauthor, Laura Esserman, M.D., a physician at the University of California, San Francisco, describe what the findings mean to women and their physicians.
“Primary care physicians, gynecologists and women need to be more aware that these tests exist,” Kaklamani said. “So if a woman has a family history of ovarian cancer or breast cancer, the woman can be genetically tested. Testing should not start with the oncologists. That’s when patients already have breast cancer. The primary care doctors and gynecologists are the ones who should evaluate patients and offer them genetic counseling.”
About 10 to 20 percent of breast and ovarian cancers are due to BRCA1 or BRCA2 genes. “Most of these women will die of ovarian cancer, so you can save 20 percent of them with the prophylactic surgery,” Kaklamani said. “And you can save the majority of women who would have died of their breast cancer.”
Even women diagnosed with breast or ovarian cancer can still benefit from genetic testing “because the presence of a mutation significantly increases the risk of a second primary (breast or ovarian) diagnosis and often influences the choice of treatments,” the authors write.
While some women diagnosed with the gene mutation may opt for surveillance with an alternating mammogram and breast magnetic resonance imaging every six months, the authors emphasize surveillance is not prevention. And, ovarian cancer screening has limited value.
Women should be aware that options for these preventive surgeries have improved, the authors note. A laparoscopic salpingo-oophorectomy is a relatively low-risk procedure and can be done in an out-patient setting. And cosmetic options for women getting mastectomies have greatly improved.
