 Free breast and cervical cancer screening is available in all 68 of the U.S. states, tribes and territories through a program that has been in existence for 20 years. The National Breast and Cervical Cancer Early Detection Program (NBCCEDP) sponsored by the Center for Disease Control and Prevention (CDC) provides access to free or low cost mammograms and Pap tests to under-insured and uninsured women. To receive services through this program, federal guidelines require a woman to be under-insured or uninsured. Each state/territory has it's own definitions for these terms. Women must be between the ages of 40 and 64 for breast cancer screening. Cervical cancer screening is also available through this program and there are some states that offer coverage for treatment if cancer is detected. An estimated 8-11% of women throughout the US are eligible to receive services. To find out if you qualify for free or low-cost mammograms and Pap tests, contact your local program by visiting http://apps.nccd.cdc.gov/cancercontacts/nbccedp/contacts.asp or call 1-800-CDC-INFO.
Free breast and cervical cancer screening is available in all 68 of the U.S. states, tribes and territories through a program that has been in existence for 20 years. The National Breast and Cervical Cancer Early Detection Program (NBCCEDP) sponsored by the Center for Disease Control and Prevention (CDC) provides access to free or low cost mammograms and Pap tests to under-insured and uninsured women. To receive services through this program, federal guidelines require a woman to be under-insured or uninsured. Each state/territory has it's own definitions for these terms. Women must be between the ages of 40 and 64 for breast cancer screening. Cervical cancer screening is also available through this program and there are some states that offer coverage for treatment if cancer is detected. An estimated 8-11% of women throughout the US are eligible to receive services. To find out if you qualify for free or low-cost mammograms and Pap tests, contact your local program by visiting http://apps.nccd.cdc.gov/cancercontacts/nbccedp/contacts.asp or call 1-800-CDC-INFO.
 In the recent Institute of Medicine report that we blogged about a week ago, Women's Health Research: Progress, Pitfalls, and Promise" it was reported that there has been a lot of progress in the areas of breast cancer, heart disease, and cervical cancer, in particularly, but less progress in areas where mortality was less of an issue than quality of life. One of those conditions that would fall into the quality of life category is Irritable Bowel Syndrome which is more common in women than in men.
In the recent Institute of Medicine report that we blogged about a week ago, Women's Health Research: Progress, Pitfalls, and Promise" it was reported that there has been a lot of progress in the areas of breast cancer, heart disease, and cervical cancer, in particularly, but less progress in areas where mortality was less of an issue than quality of life. One of those conditions that would fall into the quality of life category is Irritable Bowel Syndrome which is more common in women than in men.
The Institute for Women's Health Research focused its October 2010 monthly e-newsletter on this topic and it can be found on our website. Another article about some interesting research on IBS can be found here.
 Dr. Teresa Woodruff, Director of the Institute for Women's Health Research at Northwestern, and her colleagues have just released their second book on oncofertility. Oncofertility is a new field of study named by Dr. Woodruff who is a leader in the study of fertility preservation in women who have lost their fertility due to cancer therapies and other conditions that threaten their ability to conceive and bear children. The issue of fertility preservation is of particular concern to young breast cancer survivors and their health care team. To learn more about this book and where to find it read below.
Dr. Teresa Woodruff, Director of the Institute for Women's Health Research at Northwestern, and her colleagues have just released their second book on oncofertility. Oncofertility is a new field of study named by Dr. Woodruff who is a leader in the study of fertility preservation in women who have lost their fertility due to cancer therapies and other conditions that threaten their ability to conceive and bear children. The issue of fertility preservation is of particular concern to young breast cancer survivors and their health care team. To learn more about this book and where to find it read below.
The Oncofertility Consortium® is pleased to announce that the second volume of its Oncofertility series is now available on Amazon.com!
Fertility preservation is an emerging field not only in the basic and clinical sciences, but also in the social sciences and humanities. Oncofertility: Ethical, Legal, Social, and Medical Perspectives offers insights by experts and scholars in bioethics, philosophy, religion, communication, and history, who tackled questions such as,
“What are the Jewish, Muslim, and Catholic perspectives on oncofertility?”
“What barriers to adoption do couples with a history of cancer face?”
“What decisionmaking processes do families undergo when considering fertility preservation?”
Purchase your copy of this one-of-a-kind book to discover the answers to these questions and to learn more!
Complete your Oncofertility collection with the first volume, Oncofertility: Fertility Preservation for Cancer Survivors, also available on Amazon.com!
 On September 27, 2010, the federal Office on Research on Women's Health (ORWH) celebrated it's 20th Anniversary at the National Institutes of Health in Bethesda, MD. Several of the former or current Congressional representatives who created the legislation to establish the ORWH were present to hear a summary of the progress made in the last 20 years. In addition, the Vision for 2020 for Women's Health was presented by Dr. Vivian Pinn, the Associate Director for Research on Women's Health. This Vision was a compilation of a two year strategic planning process that included 5 regional meetings held across the country including one held at Northwestern University, home of the Institute for Women's Health Research. These meeting involved more than 1500 scientists, advocates, public policy experts, health providers and elected officials. It included published testimony from hundreds of consumers.
On September 27, 2010, the federal Office on Research on Women's Health (ORWH) celebrated it's 20th Anniversary at the National Institutes of Health in Bethesda, MD. Several of the former or current Congressional representatives who created the legislation to establish the ORWH were present to hear a summary of the progress made in the last 20 years. In addition, the Vision for 2020 for Women's Health was presented by Dr. Vivian Pinn, the Associate Director for Research on Women's Health. This Vision was a compilation of a two year strategic planning process that included 5 regional meetings held across the country including one held at Northwestern University, home of the Institute for Women's Health Research. These meeting involved more than 1500 scientists, advocates, public policy experts, health providers and elected officials. It included published testimony from hundreds of consumers.
The six goals for the future included in the strategic plan are:
1. Increase sex difference research in basic science studies.
2. Incorporate findings of sex/gender differences in the design and application of new technologies, medical devices, and therapeutic drugs.
3. Actualize personalized prevention, diagnostics, and therapeutics for girls and women.
4. Create strategic alliances and partnerships to maximize the domestic and global impact of women's health research.
5. Develop and implement new communication and social networking technologies to increase understanding and appreciation of women's health and wellness research.
6. Employ innovative strategies to build a well-trained, diverse, and vigorous women's health research workforce.
Each of these goals has a list of specific action objectives. The complete strategic plan can be reviewed by viewing ORWH_Strategic-Plan_Vol_1_508
To view the 20th Anniversary webcast click here.
 I just got back from a brief vacation in the Italian region of Emilia Romagna--the land of Parma ham, proscuitto, Pasta Bolognese and tasty hard cheeses. One of the regional specialties is a ravioli filled with spinach and ricotta covered in a butter sauce and sprinkled with parmesan cheese (Are your arteries choking yet?). I was immediately struck by the lack of overweight people despite these wonderful foods that are high in fat and quite salty. What is it about Italy that allows people to stay thin, yet eat these rich foods?
I just got back from a brief vacation in the Italian region of Emilia Romagna--the land of Parma ham, proscuitto, Pasta Bolognese and tasty hard cheeses. One of the regional specialties is a ravioli filled with spinach and ricotta covered in a butter sauce and sprinkled with parmesan cheese (Are your arteries choking yet?). I was immediately struck by the lack of overweight people despite these wonderful foods that are high in fat and quite salty. What is it about Italy that allows people to stay thin, yet eat these rich foods?
Now, I admit that this particular blog posting is not based on comparative research but rather a reflection on a brief vacation experience. I really don't know if Italians have more heart attacks than Americans---but to the watchful eye, I was struck by all the healthy "looking" people who were strolling the piazzas who were significantly thinner than the people I see walking around the malls in America. In fact, I saw almost NO overweight people.
Yes, they walk a lot, ride bicycles and spend time walking off their meals during their traditional passegiata (Lots of the men walk with their jackets thrown over their shoulders like a cape....molte elegante!). But they also eat dinner very late (after 8 pm), close their shops for a 3 hour lunch break, and enjoy their bread, wine and gelato. On the other hand, not all meals are large, there are no fast food places in the small towns, and their cups of espresso hold about a tablespoon of caffe in those cute little cups. Everything is freshly made and the small grocery stores are not lined with freezers filled with processed foods.
We spent some time with friends who lived in the community and learned that they have all their health care covered (even though taxes are high), work about 35 hours max. a week, and have 32 plus days vacation a year which they often spend in neighboring countries hiking and biking. Many of the pharmacies provide basic health care services locally. The school children play lots of sports and not everyone has a car. Trains are plentiful between cities but, in the small towns, the best way to get around is to walk. Their houses and apartments are half the size of those in America but very adequate. Their way of life seems more relaxed---everywhere you looked, people were gathered and simply enjoying each other----and talking to each other! Cell phones were plentiful but they didn't seem to replace face to face conversation. I didn't see people eating at tables and talking on their phones as much as you see here. They don't seem to watch nearly the amount of TV that Americans do. I'm sure they have the usual worries about their jobs and families but they still have a quiet zest that permeates their everyday lives. Overall, the stress level was definitely less apparent than it is in the U.S. Maybe the word I am looking for is "content". They seemed happy with their lives whether they were farmers, teachers or stay at home moms.
People say that traveling is educational. On this trip, I learned that there are lifestyles that may be different---but perhaps better-- than ours.
 Women who undergo treatment for breast cancer may be offered the possibility of reconstruction if they opt for mastectomy. This may lead to a discussion on whether or not to do reconstruction immediately during the initial surgery or delay it until any other treatments like chemotherapy are complete. Two new studies published in the September edition of the Archives of Surgery provide additional information that could influence this decision.
Women who undergo treatment for breast cancer may be offered the possibility of reconstruction if they opt for mastectomy. This may lead to a discussion on whether or not to do reconstruction immediately during the initial surgery or delay it until any other treatments like chemotherapy are complete. Two new studies published in the September edition of the Archives of Surgery provide additional information that could influence this decision.
One study finds that about half of the women who need radiation therapy after having had a mastectomy with immediate reconstruction develop complications that require additional surgery. Another study finds that chemotherapy does not affect complication rates after mastectomy and immediate reconstruction.
Dr. Rodney Pommier, professor of surgery at Knight Cancer Institute in Portland and his colleagues found that among the women who had mastectomies and who needed radiation, complications occurred in 44 percent of those who had immediate reconstruction, but only in 7 percent of those who did not have immediate reconstruction. Both scenarios, having radiation after mastectomy and having reconstruction done immediately---strongly predicted the risk of complications according to the researchers. Radiation tripled the risk, and immediate reconstruction increase the risk eightfold.
Implants had to be removed in 31 percent of patients who had radiation after mastectomy, compared to just 6 percent of those who did not have to have radiation, the researchers reported. Pommier said that these results were higher than expected and have changed his way of thinking. He now suggests that having a biopsy of the sentinel lymph node (if positive for tumor, generally indicates that radiation may be needed) would be important. Typically this sentinel node biopsy is performed during the mastectomy but it can be done as an outpatient procedure before the mastectomy and before the decision to have reconstruction is made. The determination to do radiation also depends on other factors, such as tumor size, and some surgeons may have a different opinion about the additional sentinel node surgery. There are also different reconstructive techniques that may influence outcome.
In the second study, researchers from the University of California, San Francisco, found that chemotherapy, either before or after the mastectomy and immediate reconstruction, had no bearing on complications and the need for more procedures.
To read more click here.
 A new report by the Institute of Medicine issued on Sept. 23, concludes that there has been some progress in women's health over the past two decades especially in lessening the burden of disease and reduced deaths among women in the areas of cardiovascular disease, breast cancer and cervical cancer, specifically. The effort has yielded less but still significant progress in reducing the effects of depresssion, HIV/AIDS, and osteoporosis in women. However, the report also identifies several areas that are important to women that have seen little progress, namely, unintended pregnancy, autoimmune disease, alcohol and drug addiction, lung cancer, and dementia.
A new report by the Institute of Medicine issued on Sept. 23, concludes that there has been some progress in women's health over the past two decades especially in lessening the burden of disease and reduced deaths among women in the areas of cardiovascular disease, breast cancer and cervical cancer, specifically. The effort has yielded less but still significant progress in reducing the effects of depresssion, HIV/AIDS, and osteoporosis in women. However, the report also identifies several areas that are important to women that have seen little progress, namely, unintended pregnancy, autoimmune disease, alcohol and drug addiction, lung cancer, and dementia.
Overall, few gains have been made on chronic and debilitating conditions that cause significant suffering but have lower death rates, pointing to the need for researchers to give quality of life similar consideration as mortality for research attention. The report also points out that barriers such as socio-economic and cultural influences still limit the potential reach and impact of research developments, especially among disadvantaged women.
Several observations made by the experts who wrote the report are in areas the Institute for Women's Health Research at Northwestern has raised as ongoing problems. One of those issues is the the fact that many research projects, even if they include both men and women, rarely report the results by sex. Furthermore, as pointed out in a recent paper in Nature, written by IWHR director, Teresa Woodruff, PhD, and her graduate students, scientific journals should require authors to include sex data in their publications.
Another challenge discussed in the report is how best to communicate complex research findings to the public and the media. The IWHR through it blog, website and monthly e-newsletters is striving to meet that challenge.
Over the next month or so, this blog will discuss issues in the IOM report in greater detail but in the meantime click HERE to read the press release, the entire report on line or to order a copy.

Did you know that perishable food carried in an old-fashioned brown bag can be unsafe to eat by lunchtime? Now that children and teens are back in school, it may be a good idea to take a look at how you are packing your kids' lunches. Most food experts recommend that an insulated lunch box is the best way to keep their lunches safe. Insulated boxes help maintain food at a safe temperature until lunchtime. Perishable foods such as cold cut sandwiches and yogurt , can be left out at room temperature for only 2 hours before they may become unsafe to eat. But with an insulated box and a chilled freezer gel pack , perishable food can stay cold and safe to eat until lunch. These suggestion also apply to mom and dad who bring their lunches to work. However, in many cases, parents have access to refrigerators at work, something the kids don't have.
Other safety tips:
Clean Hands: Wash your hands before preparing lunches, and remind your children to wash their hands before eating.
Freeze your juice box: When frozen they can be used as freezer packs. By lunchtime, the juice should be thawed and ready to drink.
Hot Foods: To keep hot foods hot, use an insulated thermos bottle.
Non-perishable Foods: Lunch items that don't need to be refrigerated include whole fruits and vegetables, hard cheese, canned meat and fish, chips, bread, peanut butter, jelly, pickles and mustard,
 Older men may be at risk of developing mild cognitive impairment (MCI), often a precursor to Alzheimer’s disease, earlier in life than older women, according to a study appearing today in Neurology. The study raises the question of whether there may be a gender difference in the development and progression of MCI.
Older men may be at risk of developing mild cognitive impairment (MCI), often a precursor to Alzheimer’s disease, earlier in life than older women, according to a study appearing today in Neurology. The study raises the question of whether there may be a gender difference in the development and progression of MCI.
Scientists evaluated the cognitive health of 1,969 dementia-free older people and found 16 percent showed signs of MCI, a condition usually marked by memory problems or other cognitive problems greater than those expected for their age. Prevalence was greater among the older participants, and it was consistently higher in men than women across all age ranges.
Ronald C. Petersen, Ph.D., M.D., and his team at the Mayo Clinic, Rochester, Minn., conducted the research.
"Because evidence indicates that Alzheimer's disease may cause changes in the brain one or two decades before the first symptoms appear, there is intense interest in investigating MCI and the earliest stages of cognitive decline," said National Institute on Aging (NIA) Director Richard J. Hodes, M.D. "While more research is needed, these findings indicate that we may want to investigate differences in the way men and women develop MCI, similar to the way stroke and cardiovascular disease risk factors and outcomes vary between the sexes."
The researchers conducted in-person evaluations of 1,969 randomly selected people from all 70- to 89-year-olds living in Olmsted County, Minn. Results of the study indicated that:
- Overall, MCI was more prevalent in men (19 percent) than in women (14 percent), even after adjusting for several demographic variables and clinical factors, such as hypertension and coronary artery disease.
- Of the 16 percent affected with MCI, over twice as many people had the amnestic form that usually progresses to Alzheimer’s disease and the prevalence rate was higher in men than in women.
- MCI prevalence was higher among people with the APOE e4 gene, a known risk factor for late-onset Alzheimer's, a form of the disease that usually occurs at age 65 or older.
- A greater number of years spent in school was significantly associated with decreased MCI prevalence, from 30 percent among participants with less than nine years of education to just 11 percent in those with more than 16 years of education.
- MCI prevalence was higher in participants who never married, as opposed to those currently or previously married.
The researchers noted that estimates of MCI prevalence vary in studies conducted around the world but generally fall into a range of 11 to 20 percent. The Mayo team's evaluation of participants included detailed in-person assessments that helped to capture the subtle changes in daily function that may mark the onset of MCI, Petersen said. The researchers also noted that the study’s limitations include a relatively low participation rate by Olmstead County residents and the fact that the population is predominantly white. Thus, these findings may not apply to other ethnic groups.
Source: NIH National Institute on Aging
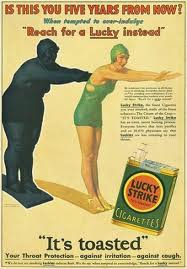
 Today,more than 200 health professionals attended the Institute for Women's Health Research at Northwestern University's first educational research forum of the 2010-2011 school year that featured Bonnie Spring, PhD, a behavioral psychologist at Northwestern. Her lecture entitled "Untangling the Web of Women, Smoking and Weight" made me realize how much we still need to learn about the power of addiction. Here are some interesting notes about smoking cessation and weight gain from her lecture:
Today,more than 200 health professionals attended the Institute for Women's Health Research at Northwestern University's first educational research forum of the 2010-2011 school year that featured Bonnie Spring, PhD, a behavioral psychologist at Northwestern. Her lecture entitled "Untangling the Web of Women, Smoking and Weight" made me realize how much we still need to learn about the power of addiction. Here are some interesting notes about smoking cessation and weight gain from her lecture:
- Reasons women continue to smoke: mood and stress management, addiction/craving, social network, weight management.
- Fear of weight gain discourages 50% of women and 26% of men who smoke from quitting. The reality is that 80% of people who quit smoking gain weight but the actual weight gain is about 6-10 lbs. , not the 15 lbs. that people assume.
- The major cause of post cessation weight gain: decreased metabolism (from nicotine cessation) and increased energy intake from snacks. Evidently, when we take away something the body values or provides pleasure (e.g., nicotine), we tend to substitute it with something else that we value (e.g. food).
- Education about the benefits of not smoking is not enough to change behavior; exercise alone to keep weight off while quitting smoking does not work.
- Drugs sometimes used during smoking cessation to keep weight down work while they are being used, but once they are stopped, the weight returns.
- Several studies have been conducted to determine if weight loss programs should be done simultaneously during smoking cessation therapy; shortly after smoking cessation has begun; or completely after the person quits. The results vary and it is not yet clear what the best approach is.
- A lot of controversy persists around the question: Do weight management efforts undermine tobacco abstinence? Despite several national guidelines that state so, there is no study that demonstrates that trying to prevent weight gain while trying to quit smoking makes it less likely that a woman will succeed at quitting smoking, according to Dr. Spring.
Some promising approaches that are being evaluated include:
- Sequential behavioral treatment (cessation, then diet and activity change) more effective than simultaneous treatment because it is less overwhelming to the patient.
- Exercise alone does not suppress weigh gain
- Bupropion, varenicline, NRT suppress weight gain in the short term, but not long-term (after medications discontinued)
- Weight acceptance (but so far tested only among very weight concerned smokers)
So the jury is still out on the best way to quit smoking. Dr. Spring also shared some of the early advertising campaigns that were highly successful in raising the number of women smokers. She noted, "Perhaps the best way to get women to quit smoking is to hire the companies that have been so successful in getting women addicted!"
