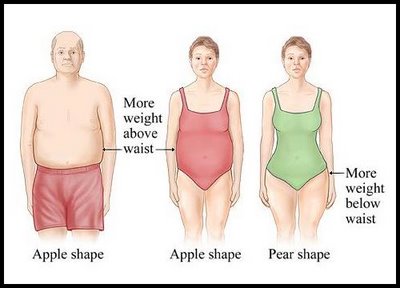
 CHICAGO --- The more an older woman weighs, the worse her memory, according to new research from Northwestern Medicine. The effect is more pronounced in women who carry excess weight around their hips, known as pear shapes, than women who carry it around their waists, called apple shapes. The study of 8,745 cognitively normal, post-menopausal women ages 65 to 79 from the Women's Health Initiative hormone trials is the first in the United States to link obesity to poorer memory and brain function in women and to identify the body-shape connection.
CHICAGO --- The more an older woman weighs, the worse her memory, according to new research from Northwestern Medicine. The effect is more pronounced in women who carry excess weight around their hips, known as pear shapes, than women who carry it around their waists, called apple shapes. The study of 8,745 cognitively normal, post-menopausal women ages 65 to 79 from the Women's Health Initiative hormone trials is the first in the United States to link obesity to poorer memory and brain function in women and to identify the body-shape connection.
"The message is obesity and a higher Body Mass Index (BMI) are not good for your cognition and your memory," said lead author Diana Kerwin M.D., an assistant professor of medicine and a physician at Northwestern Medicine. "While the women's scores were still in the normal range, the added weight definitely had a detrimental effect."
For every one-point increase in a woman's BMI, her memory score dropped by one point. The women were scored on a 100-point memory test, called the Modified Mini-Mental Status Examination. The study controlled for such variables as diabetes, heart disease and stroke. The study will be published July 14 in the Journal of the American Geriatric Society.
The reason pear-shaped women experienced more memory and brain function deterioration than apple-shaped women is likely related to the type of fat deposited around the hips versus the waist. "Obesity is bad, but its effects are worse depending on where the fat is located," Kerwin said.
Cytokines, hormones released by the predominant kind of fat in the body that can cause inflammation, likely affect cognition, Kerwin said. Scientists already know different kinds of fat release different cytokines and have different effects on insulin resistance, lipids and blood pressure.
"We need to find out if one kind of fat is more detrimental than the other, and how it affects brain function," she said. "The fat may contribute to the formation of plaques associated with Alzheimer's disease or a restricted blood flow to the brain." In the meantime, the new findings provide guidance to physicians with overweight, older female patients.
"The study tells us if we have a woman in our office, and we know from her waist-to-hip ratio that she's carrying excess fat on her hips, we might be more aggressive with weight loss," Kerwin said. "We can't change where your fat is located, but having less of it is better."
Kerwin's research is funded by the T. Franklin Williams Award from Atlantic Philanthropies and Association of Specialty Professors and the Wisconsin Women's Health Foundation Faculty Scholar Award. The Women's Health Initiative was funded by a grant from the National Heart, Lung and Blood Institute.

 Fish and shellfish are an important part of a healthy diet. They contain protein and other essential nutrients, are low in saturated fat, and contain omega-3 fatty acids. A well-balanced diet that includes a variety of seafood can contribute to heart health and children’s proper growth and development.
Fish and shellfish are an important part of a healthy diet. They contain protein and other essential nutrients, are low in saturated fat, and contain omega-3 fatty acids. A well-balanced diet that includes a variety of seafood can contribute to heart health and children’s proper growth and development.
 Several Northwestern researchers, including our own
Several Northwestern researchers, including our own 
 Women who measure their peak heart rates for exercise will need to do some new math, as will physicians giving stress tests to patients. A new formula based on a large study from Northwestern Medicine provides a more accurate estimate of the peak heart rate a healthy woman should attain during exercise. It also will more accurately predict the risk of heart-related death during a stress test.
Women who measure their peak heart rates for exercise will need to do some new math, as will physicians giving stress tests to patients. A new formula based on a large study from Northwestern Medicine provides a more accurate estimate of the peak heart rate a healthy woman should attain during exercise. It also will more accurately predict the risk of heart-related death during a stress test.