 Older men may be at risk of developing mild cognitive impairment (MCI), often a precursor to Alzheimer’s disease, earlier in life than older women, according to a study appearing today in Neurology. The study raises the question of whether there may be a gender difference in the development and progression of MCI.
Older men may be at risk of developing mild cognitive impairment (MCI), often a precursor to Alzheimer’s disease, earlier in life than older women, according to a study appearing today in Neurology. The study raises the question of whether there may be a gender difference in the development and progression of MCI.
Scientists evaluated the cognitive health of 1,969 dementia-free older people and found 16 percent showed signs of MCI, a condition usually marked by memory problems or other cognitive problems greater than those expected for their age. Prevalence was greater among the older participants, and it was consistently higher in men than women across all age ranges.
Ronald C. Petersen, Ph.D., M.D., and his team at the Mayo Clinic, Rochester, Minn., conducted the research.
"Because evidence indicates that Alzheimer's disease may cause changes in the brain one or two decades before the first symptoms appear, there is intense interest in investigating MCI and the earliest stages of cognitive decline," said National Institute on Aging (NIA) Director Richard J. Hodes, M.D. "While more research is needed, these findings indicate that we may want to investigate differences in the way men and women develop MCI, similar to the way stroke and cardiovascular disease risk factors and outcomes vary between the sexes."
The researchers conducted in-person evaluations of 1,969 randomly selected people from all 70- to 89-year-olds living in Olmsted County, Minn. Results of the study indicated that:
- Overall, MCI was more prevalent in men (19 percent) than in women (14 percent), even after adjusting for several demographic variables and clinical factors, such as hypertension and coronary artery disease.
- Of the 16 percent affected with MCI, over twice as many people had the amnestic form that usually progresses to Alzheimer’s disease and the prevalence rate was higher in men than in women.
- MCI prevalence was higher among people with the APOE e4 gene, a known risk factor for late-onset Alzheimer's, a form of the disease that usually occurs at age 65 or older.
- A greater number of years spent in school was significantly associated with decreased MCI prevalence, from 30 percent among participants with less than nine years of education to just 11 percent in those with more than 16 years of education.
- MCI prevalence was higher in participants who never married, as opposed to those currently or previously married.
The researchers noted that estimates of MCI prevalence vary in studies conducted around the world but generally fall into a range of 11 to 20 percent. The Mayo team's evaluation of participants included detailed in-person assessments that helped to capture the subtle changes in daily function that may mark the onset of MCI, Petersen said. The researchers also noted that the study’s limitations include a relatively low participation rate by Olmstead County residents and the fact that the population is predominantly white. Thus, these findings may not apply to other ethnic groups.
Source: NIH National Institute on Aging

 The millions of middle-aged and older adults who suffer from insomnia have a new drug-free prescription for a more restful night’s sleep. Regular aerobic exercise improves the quality of sleep, mood and vitality, according to a small but significant new study from Northwestern Medicine and the Feinberg School of Medicine. Insomnia is more prevalent in women.
The millions of middle-aged and older adults who suffer from insomnia have a new drug-free prescription for a more restful night’s sleep. Regular aerobic exercise improves the quality of sleep, mood and vitality, according to a small but significant new study from Northwestern Medicine and the Feinberg School of Medicine. Insomnia is more prevalent in women. An understanding why women experience more stress-related mental disorders like depression and Post Traumatic Stress Disorder (PTSD) has eluded scientists but a new study in rat brains may help explain why women are more prone to mood and anxiety disorders than men.
An understanding why women experience more stress-related mental disorders like depression and Post Traumatic Stress Disorder (PTSD) has eluded scientists but a new study in rat brains may help explain why women are more prone to mood and anxiety disorders than men. The National Institutes of Health Office of Research on Women's Health (ORWH) will celebrate its 20th anniversary with a day-long symposium on Monday, Sept. 27, in Bethesda, Maryland. Discussed will be highlights of early accomplishments in women's health research, as well as a preview of the next decade A Vision for the Year 2020. Many of the advances involve medical differences between women and men, and implications for sex/gender — appropriate clinical care and personalized medicine.
The National Institutes of Health Office of Research on Women's Health (ORWH) will celebrate its 20th anniversary with a day-long symposium on Monday, Sept. 27, in Bethesda, Maryland. Discussed will be highlights of early accomplishments in women's health research, as well as a preview of the next decade A Vision for the Year 2020. Many of the advances involve medical differences between women and men, and implications for sex/gender — appropriate clinical care and personalized medicine. Women with the most serious type of angina are three times as likely as men with the same condition to develop severe coronary artery disease (CAD), researchers have found.
Women with the most serious type of angina are three times as likely as men with the same condition to develop severe coronary artery disease (CAD), researchers have found. In 2006, the Center for Disease Control and Prevention (CDC) reported that 21.6% of the US adult population reported arthritis, with significantly higher prevalence in women than in men (24.4% vs. 18.1%). Arthritis prevalence increased with age and was higher among women than men in every age group. With the aging of the US population, the prevalence of doctor-diagnosed arthritis is expected to increase in the coming decades. By 2030, it is estimated that 67 million adults age 18 and older will have arthritis, compared with the current 46 million. Also, by 2030 an estimated 25 million adults will report arthritis-attributable activity limitations.
In 2006, the Center for Disease Control and Prevention (CDC) reported that 21.6% of the US adult population reported arthritis, with significantly higher prevalence in women than in men (24.4% vs. 18.1%). Arthritis prevalence increased with age and was higher among women than men in every age group. With the aging of the US population, the prevalence of doctor-diagnosed arthritis is expected to increase in the coming decades. By 2030, it is estimated that 67 million adults age 18 and older will have arthritis, compared with the current 46 million. Also, by 2030 an estimated 25 million adults will report arthritis-attributable activity limitations. No, you did not open the wrong page. Yes, this blog is posted by the
No, you did not open the wrong page. Yes, this blog is posted by the  Low testosterone levels to blame for low libido, fatigue and weight gain
Low testosterone levels to blame for low libido, fatigue and weight gain All living organisms have a circadian clock, sometimes called a biological clock, that is an important part of maintaining optimal health. The circadian rhythm is a roughly 24-hour cycle in the biochemical, physiological, or behavioral processes of living things. Although circadian rhythms originate from within our bodies, they are synchronized to the environment by external cues, including the day-night cycle caused by the Earth's rotation. Researchers are looking more closely at the role circadian rhythms play in the development of diseases such as breast cancer and also how factors such as hormones affect this biological clock.
All living organisms have a circadian clock, sometimes called a biological clock, that is an important part of maintaining optimal health. The circadian rhythm is a roughly 24-hour cycle in the biochemical, physiological, or behavioral processes of living things. Although circadian rhythms originate from within our bodies, they are synchronized to the environment by external cues, including the day-night cycle caused by the Earth's rotation. Researchers are looking more closely at the role circadian rhythms play in the development of diseases such as breast cancer and also how factors such as hormones affect this biological clock.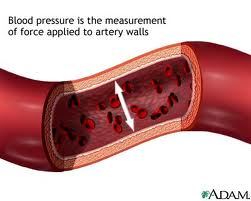 Postmenopausal women have an increased risk of hypertension (high blood pressure), and among older adults, more women than men have hypertension. As with many other health issues, hypertension research has been conducted predominately in males, and little is known about how women's bodies manage blood flow. Research conducted by Heidi A. Kluess at the University of Arkansas is focusing on a better understanding of hypertension in women by using a new technique to examine the release of a neurotransmitter in small blood vessels.
Postmenopausal women have an increased risk of hypertension (high blood pressure), and among older adults, more women than men have hypertension. As with many other health issues, hypertension research has been conducted predominately in males, and little is known about how women's bodies manage blood flow. Research conducted by Heidi A. Kluess at the University of Arkansas is focusing on a better understanding of hypertension in women by using a new technique to examine the release of a neurotransmitter in small blood vessels. Several Northwestern researchers, including our own
Several Northwestern researchers, including our own