 People will gain significantly less weight by middle age – especially women – if they engage in moderate to vigorous activity nearly every day of the week starting as young adults, according to new Northwestern Medicine research.
People will gain significantly less weight by middle age – especially women – if they engage in moderate to vigorous activity nearly every day of the week starting as young adults, according to new Northwestern Medicine research.
Women particularly benefitted from high activity over 20 years, gaining an average of 13 pounds less than those with low activity; while men with high activity gained about 6 pounds less than their low-activity peers. High activity included recreational exercise such as basketball, running, brisk walking or an exercise class or daily activities such as housework or construction work.
“Everyone benefits from high activity, but I was surprised by the gender differences,” said lead author Arlene Hankinson, M.D., an instructor in preventive medicine at Northwestern University Feinberg School of Medicine. “It wasn’t that activity didn’t have an effect in men, but the effect was greater in women. Now women should be especially motivated.”
The study will be published Dec. 14 in the Journal of the American Medical Association.
There could be several reasons for the gender difference, Hankinson said. Women are less likely than men to overestimate their activity, according to previous studies. “Men may not be getting as much activity as they report,” Hankinson explained. In addition, men in the high-activity group compensated by eating more than their low-activity counterparts, which could have led to more weight gain. The highly active women didn’t eat more than low-activity women in the study.
There were many ways to achieve the study’s definition of high-activity levels, Hankinson noted. One way was 150 minutes of moderate to vigorous activity a week.
The study participants -- 1,800 women and nearly 1,700 men — are part of the Coronary Artery Risk Development in Young Adults (CARDIA) Study, a multi-center, longitudinal and population-based observational study designed to describe the development of risk factors for coronary heart disease in young black and white adults.
Coauthor Stephen Sidney, M.D., associate director for clinical research at the Kaiser Permanente Division of Research. “Common medical problems such as heart disease, diabetes and obesity have their origins in childhood and can generally be prevented by maintaining a normal weight, not smoking, exercising regularly and eating a healthy diet throughout life.”
Hankinson’s research is the first to measure the impact of high activity over 20 years between young adulthood and middle age and to frequently examine participants (seven times) over that period. Study participants are more likely to remember and accurately report their behavior with regular exams, she said. Previous studies, Hankinson said, looked at a single exercise intervention’s effect on weight for a short period of time or examined participants in longer studies at only two points in time -– the beginning and the end.
“We wanted to see if people’s activity levels during their youth were enough to help them keep weight off in middle age, or if they needed to up the ante,” Hankinson said. “It’s difficult to avoid gaining weight as you age. Our metabolic rate goes down. We develop conditions or have lifestyles that make it harder to maintain a high level of activity.”
“The study reinforces that everyone needs to make regular activity part of their lifestyles throughout their lives,” she said. “Not many people actually do that.” The active group in the study comprised only 12 percent of the participants. Lower levels of activity had a negligible effect on weight gain in the study. “High activity was the only kind that made a significant difference,” Hankinson noted.

 Working mothers are two-and-a-half times as likely as working fathers to interrupt their sleep to take care of others.
Working mothers are two-and-a-half times as likely as working fathers to interrupt their sleep to take care of others. Alzheimer's disease affects twice as many women as it does men, according to a new report that portrays women as being "under siege" by the dreaded condition.
Alzheimer's disease affects twice as many women as it does men, according to a new report that portrays women as being "under siege" by the dreaded condition. In celebration of National Diabetes Awareness Month, the
In celebration of National Diabetes Awareness Month, the  Between 2000 and 2007, the death rate of men treated in hospitals for stroke tumbled by 29 percent compared to a 24 percent decline for women, according to the latest News and Numbers from the Agency for Healthcare Research and Quality (AHRQ).
Between 2000 and 2007, the death rate of men treated in hospitals for stroke tumbled by 29 percent compared to a 24 percent decline for women, according to the latest News and Numbers from the Agency for Healthcare Research and Quality (AHRQ).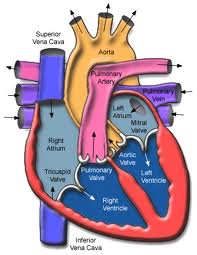
 In the recent Institute of Medicine report that we blogged about a week ago,
In the recent Institute of Medicine report that we blogged about a week ago,  On September 27, 2010, the federal Office on Research on Women's Health (ORWH) celebrated it's 20th Anniversary at the National Institutes of Health in Bethesda, MD. Several of the former or current Congressional representatives who created the legislation to establish the ORWH were present to hear a summary of the progress made in the last 20 years. In addition, the Vision for 2020 for Women's Health was presented by Dr. Vivian Pinn, the Associate Director for Research on Women's Health. This Vision was a compilation of a two year strategic planning process that included 5 regional meetings held across the country including one held at Northwestern University, home of the Institute for Women's Health Research. These meeting involved more than 1500 scientists, advocates, public policy experts, health providers and elected officials. It included published testimony from hundreds of consumers.
On September 27, 2010, the federal Office on Research on Women's Health (ORWH) celebrated it's 20th Anniversary at the National Institutes of Health in Bethesda, MD. Several of the former or current Congressional representatives who created the legislation to establish the ORWH were present to hear a summary of the progress made in the last 20 years. In addition, the Vision for 2020 for Women's Health was presented by Dr. Vivian Pinn, the Associate Director for Research on Women's Health. This Vision was a compilation of a two year strategic planning process that included 5 regional meetings held across the country including one held at Northwestern University, home of the Institute for Women's Health Research. These meeting involved more than 1500 scientists, advocates, public policy experts, health providers and elected officials. It included published testimony from hundreds of consumers. A new report by the Institute of Medicine issued on Sept. 23, concludes that there has been some progress in women's health over the past two decades especially in lessening the burden of disease and reduced deaths among women in the areas of cardiovascular disease, breast cancer and cervical cancer, specifically. The effort has yielded less but still significant progress in reducing the effects of depresssion, HIV/AIDS, and osteoporosis in women. However, the report also identifies several areas that are important to women that have seen little progress, namely, unintended pregnancy, autoimmune disease, alcohol and drug addiction, lung cancer, and dementia.
A new report by the Institute of Medicine issued on Sept. 23, concludes that there has been some progress in women's health over the past two decades especially in lessening the burden of disease and reduced deaths among women in the areas of cardiovascular disease, breast cancer and cervical cancer, specifically. The effort has yielded less but still significant progress in reducing the effects of depresssion, HIV/AIDS, and osteoporosis in women. However, the report also identifies several areas that are important to women that have seen little progress, namely, unintended pregnancy, autoimmune disease, alcohol and drug addiction, lung cancer, and dementia.