 Eating fish at least once a week could help lower older patients' risk of developing dementia, according to Cyrus Raji, MD, PhD, from the University of Pittsburgh and colleagues reported at the Nov. 2011 Radiological Society of North America meeting.
Eating fish at least once a week could help lower older patients' risk of developing dementia, according to Cyrus Raji, MD, PhD, from the University of Pittsburgh and colleagues reported at the Nov. 2011 Radiological Society of North America meeting.
Those who ate baked or broiled -- but not fried -- fish on a weekly basis had a greater volume of gray matter in areas of the brain associated with Alzheimer's disease than people who didn't eat fish as often. Preserving brain volume was also associated with lower rates of developing cognitive impairment, he said.
"Fish consumption benefits gray matter volume, potentially reducing the risk of [Alzheimer's disease and dementia] long-term," Raji said during a press briefing.
Although a National Institutes of Health panel decided last year that nothing conclusively prevents Alzheimer's disease, researchers continue to investigate whether a healthy diet, or specific components thereof, can have any beneficial effects.
For their study, Raji and colleagues assessed 260 people, mean age 71, when they enrolled in the Cardiovascular Health Study between 1989 and 1990. At that time, they filled out questionnaires on dietary intake; 163 reported eating fish at least weekly, and some did so as often as four times a week.
All patients had an MRI 10 years later to assess brain volume, and then had follow-up cognitive testing between 2002 and 2003.
The researchers found that patients who ate fish at least once a week had greater volume in the frontal lobes and the temporal lobes, areas responsible for memory and learning, which are severely affected in Alzheimer's disease, Raji said.
Five years after the MRI, they found that 30.8% of patients who had low fish intake had developed mild cognitive impairment or dementia, compared with just 3.2% of those who had the highest fish intake and the greatest preservation of brain volume.
They also saw that 47% of patients with brain atrophy who didn't eat fish had abnormal cognition five years later compared with 28% of those who ate more fish and had more gray matter volume, Raji reported. "That's an impressive reduction in the risk of developing mild cognitive impairment of Alzheimer's," Raji said.
In further analyses, the researchers found that mean scores for working memory -- a function severely impaired in Alzheimer's disease -- were significantly higher among those who ate fish weekly and those findings persisted even after accounting for potential confounders.
This "simple lifestyle choice" of eating more fish increases the brain's "resistance" to Alzheimer's disease, Raji said, potentially via a few mechanisms: Fish are rich in omega-3 fatty acids, which can help increase blood flow to the brain and can also act as an antioxidant, thereby reducing inflammation, he said.
Omega-3s may also prevent the accumulation of amyloid plaques in the brain, he added. He noted that fatty fish like salmon have more omega-3s, while smaller fish, such as cod, have less.
Although dietary intake of fish was measured only twice -- once at baseline and again in 1995 -- Raji said patients tended to maintain their levels of consumption, and he suspects that the observed benefits "are more likely to be observed if eating fish is a long-term habit as opposed to a short-term approach."
Mary Mahoney, MD, of the University of Cincinnati, who was not involved in the study, said that future studies should investigate whether omega-3s specifically are leading to benefits in brain volume.
"We're making the assumption" that fish is a marker for healthy lifestyle, she said. "If we could just cut to the chase and look at the protective mechanism, that would be better."
It's important to note that the findings are preliminary and should be replicated in a larger sample and sex differences should be included since Altzeimer's is more prevalent in women. In the meantime, it can't hurt to add fish to your diet...for many reasons!
Source reference:
Raji C, et al "Fish consumption, brain structure, and risk of Alzheimer's disease" RSNA 2011.
 Today, I walked by a filled meeting room and overheard someone say, " I never open my paper mail any more." It sounded like the group was discussing email banking and other electronic transactions. Though I still pay my bills by snail mail, I recognize the potential benefits of the latest phone and computer apps--I'm just not ready for it! Email and facebook has reconnected families and opened communications lines that enable busy, overworked people to keep you posted on their latest activities.
Today, I walked by a filled meeting room and overheard someone say, " I never open my paper mail any more." It sounded like the group was discussing email banking and other electronic transactions. Though I still pay my bills by snail mail, I recognize the potential benefits of the latest phone and computer apps--I'm just not ready for it! Email and facebook has reconnected families and opened communications lines that enable busy, overworked people to keep you posted on their latest activities.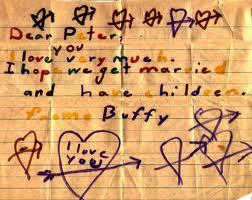 What does concern me is the loss of the wonderful art of letterwriting. Does anyone remember when love letters were saved and tied in ribbon? What about those letters you received at camp or when you first went away to college? The handwritten letter meant someone was really thinking about you and missed you. The letter was even more special if the writing itself was beautiful or if the bold print of a child was accompanied by a colorful crayola picture! Today, many of us still find old letters in boxes that are stored away in our sheds and closets from families and friends. Somehow, opening a computer file just doesn't work quite the same when it comes to nostalgia and fond memories.
What does concern me is the loss of the wonderful art of letterwriting. Does anyone remember when love letters were saved and tied in ribbon? What about those letters you received at camp or when you first went away to college? The handwritten letter meant someone was really thinking about you and missed you. The letter was even more special if the writing itself was beautiful or if the bold print of a child was accompanied by a colorful crayola picture! Today, many of us still find old letters in boxes that are stored away in our sheds and closets from families and friends. Somehow, opening a computer file just doesn't work quite the same when it comes to nostalgia and fond memories.
 This time of year, the shorter days and lack of sunlight can cause some people to feel depressed. Seasonal Affective Disorder, or SAD, affects between 10 to 20 percent of Americans, primarily younger adults and women. Although the exact cause of SAD is unknown, experts believe changes in melatonin and serotonin levels, or a disruption in the body’s internal clock may be to blame. John Stracks, MD, from Northwestern Integrative Medicine says there are ways to beat the blues caused by SAD and suggests those who experience symptoms visit their doctor before symptoms become severe.
This time of year, the shorter days and lack of sunlight can cause some people to feel depressed. Seasonal Affective Disorder, or SAD, affects between 10 to 20 percent of Americans, primarily younger adults and women. Although the exact cause of SAD is unknown, experts believe changes in melatonin and serotonin levels, or a disruption in the body’s internal clock may be to blame. John Stracks, MD, from Northwestern Integrative Medicine says there are ways to beat the blues caused by SAD and suggests those who experience symptoms visit their doctor before symptoms become severe. Some people don’t take food poisoning very seriously. Maybe that’s because the symptoms usually are not long-lasting in most healthy people—a few hours or a few days—and usually go away without medical treatment. But foodborne illness can be severe, even life-threatening to anyone, especially those most at risk such as older adults, infants and young children, pregnant women, and people with HIV/AIDS, cancer, or any condition that weakens their immune systems.
Some people don’t take food poisoning very seriously. Maybe that’s because the symptoms usually are not long-lasting in most healthy people—a few hours or a few days—and usually go away without medical treatment. But foodborne illness can be severe, even life-threatening to anyone, especially those most at risk such as older adults, infants and young children, pregnant women, and people with HIV/AIDS, cancer, or any condition that weakens their immune systems. Clean: Resolve to wash your hands before, during and after handling food. According to the Centers for Disease Control and Prevention (CDC), handwashing has the potential to save more lives than any single vaccine or medical intervention. To do it effectively, wet your hands with clean running water (warm or cold) and apply soap. Rub your hands together to make a lather and scrub them well for at least 20 seconds. Air dry or use a clean paper towel.
Clean: Resolve to wash your hands before, during and after handling food. According to the Centers for Disease Control and Prevention (CDC), handwashing has the potential to save more lives than any single vaccine or medical intervention. To do it effectively, wet your hands with clean running water (warm or cold) and apply soap. Rub your hands together to make a lather and scrub them well for at least 20 seconds. Air dry or use a clean paper towel. Cook: Resolve to get a food thermometer, if you don’t have one. Only a food thermometer can make sure meat, poultry, fish, and casseroles are cooked to a safe internal temperature—hot enough to kill any pathogens that may be present.
Cook: Resolve to get a food thermometer, if you don’t have one. Only a food thermometer can make sure meat, poultry, fish, and casseroles are cooked to a safe internal temperature—hot enough to kill any pathogens that may be present. Women and men between the ages of 45 and 64 were more than twice as likely to have had knee replacement surgery in 2009 than in 1997, recent data from the Agency for Healthcare Research and Quality (AHRQ) show. The rates among women were even higher. Knee replacement surgery is most common in people whose knees have been damaged by osteoarthritis (OA), rheumatoid arthritis, or injury. Due to their age and fondness for sports, Baby Boomers fit neatly into each category.
Women and men between the ages of 45 and 64 were more than twice as likely to have had knee replacement surgery in 2009 than in 1997, recent data from the Agency for Healthcare Research and Quality (AHRQ) show. The rates among women were even higher. Knee replacement surgery is most common in people whose knees have been damaged by osteoarthritis (OA), rheumatoid arthritis, or injury. Due to their age and fondness for sports, Baby Boomers fit neatly into each category. Eating fish at least once a week could help lower older patients' risk of developing dementia, according to Cyrus Raji, MD, PhD, from the University of Pittsburgh and colleagues reported at the Nov. 2011 Radiological Society of North America meeting.
Eating fish at least once a week could help lower older patients' risk of developing dementia, according to Cyrus Raji, MD, PhD, from the University of Pittsburgh and colleagues reported at the Nov. 2011 Radiological Society of North America meeting. A hike in your blood pressure during middle age significantly raises the risk of having a heart attack or a stroke during your lifetime, according to new Northwestern Medicine research. The study offers a new understanding on the importance of maintaining low blood pressure early in middle age to prevent heart disease later in life. Men and women who developed high blood pressure in middle age or who started out with high blood pressure had an estimated 30 percent increased risk of having a heart attack or stroke compared to those who kept their blood pressure low.
A hike in your blood pressure during middle age significantly raises the risk of having a heart attack or a stroke during your lifetime, according to new Northwestern Medicine research. The study offers a new understanding on the importance of maintaining low blood pressure early in middle age to prevent heart disease later in life. Men and women who developed high blood pressure in middle age or who started out with high blood pressure had an estimated 30 percent increased risk of having a heart attack or stroke compared to those who kept their blood pressure low. Remember when road rage was mainly triggered by rush hour traffic? Recently, I was driving in local traffic near the university when a car in front of me was signaling left and made a sudden move to the RIGHT lane. Okay, we all get confused. In the next block the driver all of a sudden moved to the middle of the road between two lanes. I slammed on my brakes and honked my horn. When the driver finally pulled into one lane, I moved up and saw the elderly woman driver clearly on her cell phone. She looked at me as I motioned "get off your phone" and I don't think she had a clue why I was signaling her. Within two city blocks I could have not one, but two accidents. Distracted driving is a dangerous and common practice, especially as more drivers are not just talking, they are texting. According to the National Highway Traffic Safety Administration, more than 3000 people died in car accidents in 2010 because drivers were texting, on the phone, or were distracted by something else like eating, putting on makeup, etc. Here are a few more stats:
Remember when road rage was mainly triggered by rush hour traffic? Recently, I was driving in local traffic near the university when a car in front of me was signaling left and made a sudden move to the RIGHT lane. Okay, we all get confused. In the next block the driver all of a sudden moved to the middle of the road between two lanes. I slammed on my brakes and honked my horn. When the driver finally pulled into one lane, I moved up and saw the elderly woman driver clearly on her cell phone. She looked at me as I motioned "get off your phone" and I don't think she had a clue why I was signaling her. Within two city blocks I could have not one, but two accidents. Distracted driving is a dangerous and common practice, especially as more drivers are not just talking, they are texting. According to the National Highway Traffic Safety Administration, more than 3000 people died in car accidents in 2010 because drivers were texting, on the phone, or were distracted by something else like eating, putting on makeup, etc. Here are a few more stats: Half of all stillbirths result from pregnancy disorders and conditions that affect the placenta, according to a new report. Risk factors already known at the start of pregnancy—such as previous pregnancy loss or obesity—accounted for only a small proportion of the overall risk of stillbirth.
Half of all stillbirths result from pregnancy disorders and conditions that affect the placenta, according to a new report. Risk factors already known at the start of pregnancy—such as previous pregnancy loss or obesity—accounted for only a small proportion of the overall risk of stillbirth. Why do so many postmenopausal women who are treated for estrogen-sensitive breast cancer quit using drugs that help prevent the disease from recurring?
Why do so many postmenopausal women who are treated for estrogen-sensitive breast cancer quit using drugs that help prevent the disease from recurring?