Epidemiological studies have shown female shift workers, such as nurses, and female flight attendants who work on long-distance east-west routes (i.e., those with constant jet lag) have fertility and menstrual issues. They are habitually out of sync with the external light cycle. But the role circadian rhythm disruption may play in their reproductive problems is a poorly studied area.
Research led by Northwestern U. circadian rhythm expert Fred W. Turek now draws a clear line between disrupted circadian rhythms and reproductive physiology. Turek and his colleagues are the first to show that if you disrupt the circadian clock environmentally in mice, with repeated changes in their light-dark cycles, there are problems with pregnancy outcomes.
And the effect can be dramatic. The researchers found evidence suggesting the severity of circadian disruption may be linked to the severity of pregnancy disruption: mice subjected to advances of the light-dark cycle had greater circadian clock disruption and lower reproductive success. This group’s pregnancy success rate was only 22 percent.
The study was published today in the journal PLoS ONE.
“Our results have important implications for the reproductive health of female shift workers, women with circadian rhythm sleep disorders and/or women with disturbed circadian rhythms for other reasons,” Turek said.
“If you disrupt your internal rhythms, there will be negative consequences -- that is very clear,” said Keith Summa, first author of the paper and an M.D./Ph.D. candidate working in Turek’s lab. “Our results suggest people should consider their biological rhythms for optimal health.”
The repeated shifting of the light-dark cycle shifts the biological clock throughout the body. This environmental disturbance is more relevant to shift workers and those frequently flying across time zones, the researchers note, than genetic disruption of the circadian clock, which also negatively influences reproductive function.
Turek, Summa and their colleague and co-author Martha H. Vitaterna studied three sets of normal laboratory female mice, all who had recently mated. The study was conducted over the course of 21 days, the duration of a typical pregnancy.
One set was a control group of 12 mice that experienced normal days of 12 hours of light, followed by 12 hours of darkness. The two other groups, of 18 mice each, also experienced days of 12 hours of light and 12 hours of darkness. But the phase-advanced group had its 12 hours of light start six hours earlier every five days. The phase-delayed group had its light start six hours later every five days. (There were a total of four phase shifts over the duration of the study.)
The researchers monitored the mice throughout the gestation period to count the number of full-term pregnancies. The results surprised them.
In the control mice, 90 percent of the matings led to full-term pregnancies. But in the phase-delay group, the pregnancy success rate was 50 percent, while in the phase-advanced group, it was only 22 percent.
“We were surprised at how dramatic the effect of manipulating the light-dark cycle was, especially in the phase-advanced group,” Summa said. “We expected a negative effect from the circadian clock disruption, but not this much.”
They next looked at a separate group of females in the phase-delay and phase-advance protocol to see how the animals responded to the repeated phase shifts. The researchers found the phase-advanced animals required one to two days longer, on average, to return to normal rhythms. This suggests the magnitude of circadian disruption is associated with the severity of pregnancy loss.
The next steps, the researchers say, are to identify specifically the stage at which pregnancy is affected and to understand exactly how circadian disruption results in the observed adverse effects.
“We’ve made an interesting observation, but what’s causing the reduced fertility?” Summa said. “We would like to determine where exactly the phase shifts and internal rhythm disruptions are having an effect.”
The March of Dimes Foundation and the Institute for Women’s Health Research at Northwestern University (the sponsor of this blog) supported the research.
The paper is titled “Environmental Perturbation of the Circadian Clock Disrupts Pregnancy in the Mouse.”
 The Centers for Disease Control and Prevention released the final version of its National Public Health Action Plan for the Detection, Prevention and Management of Infertility. The National Action Plan developed over the course of seven years and began with an ad hoc working group that included members of the Oncofertility Consortium that started at Northwestern. A draft National Action Plan was released in May 2012. ASRM provided input at each step of process under which the National Action Plan was developed and will continue to be involved as the National Action Plan is implemented.
The Centers for Disease Control and Prevention released the final version of its National Public Health Action Plan for the Detection, Prevention and Management of Infertility. The National Action Plan developed over the course of seven years and began with an ad hoc working group that included members of the Oncofertility Consortium that started at Northwestern. A draft National Action Plan was released in May 2012. ASRM provided input at each step of process under which the National Action Plan was developed and will continue to be involved as the National Action Plan is implemented.
 Acupuncture has been used in Eastern countries to address women's health issues but is not readily adopted in the U.S. especially by the medical establishment. A new study reports preliminary data indicating that acupuncture may improve menstrual health and overcome delays in becoming pregnant. There are experimental data indicating that acupuncture can influence female reproductive functioning, although the actual mechanisms involved are not yet clarified. Acupuncture is a complex intervention yet the evaluation of acupuncture research designs and outcome measures expect a level of commensurability difficult to achieve in complex interventions. A focus on effectiveness rather than efficacy may be a solution. Further research is needed that includes the rich traditions of acupuncture practice and the rigorous methods of evidence-based research.
Acupuncture has been used in Eastern countries to address women's health issues but is not readily adopted in the U.S. especially by the medical establishment. A new study reports preliminary data indicating that acupuncture may improve menstrual health and overcome delays in becoming pregnant. There are experimental data indicating that acupuncture can influence female reproductive functioning, although the actual mechanisms involved are not yet clarified. Acupuncture is a complex intervention yet the evaluation of acupuncture research designs and outcome measures expect a level of commensurability difficult to achieve in complex interventions. A focus on effectiveness rather than efficacy may be a solution. Further research is needed that includes the rich traditions of acupuncture practice and the rigorous methods of evidence-based research. I think women want to feel independent, that we can conquer the world on our own. Sometimes it can be hard to ask for help.
I think women want to feel independent, that we can conquer the world on our own. Sometimes it can be hard to ask for help. A new study shows that the biological clock is not the only clock women trying to conceive should consider. The
A new study shows that the biological clock is not the only clock women trying to conceive should consider. The  Just 38 percent of sexually active young women were screened for
Just 38 percent of sexually active young women were screened for 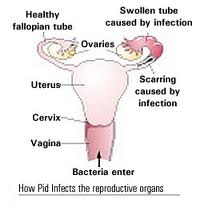 Pelvic inflammatory disease (PID) refers to infection of the uterus (womb), fallopian tubes and other reproductive organs that causes symptoms such as lower abdominal pain. It is a serious complication of some sexually transmitted diseases, especially chlamydia and gonorrhea. PID can damage the fallopian tubes and tissues in and near the uterus and ovaries and can lead to serious consequences including infertility, ectopic pregnancy (a pregnancy in the fallopian tube or elsewhere outside the womb), abscess formation and chronic pelvic pain.
Pelvic inflammatory disease (PID) refers to infection of the uterus (womb), fallopian tubes and other reproductive organs that causes symptoms such as lower abdominal pain. It is a serious complication of some sexually transmitted diseases, especially chlamydia and gonorrhea. PID can damage the fallopian tubes and tissues in and near the uterus and ovaries and can lead to serious consequences including infertility, ectopic pregnancy (a pregnancy in the fallopian tube or elsewhere outside the womb), abscess formation and chronic pelvic pain. For some unknown reason, we are suddenly receiving a lot of comments on our March 2010 posting on Endometriosis. Maybe it is because endometriosis is one of the most common gynecological diseases, affecting more that 5.5 million women in North America alone. There is a comprehensive fact sheet available from the National Institute of Child Health and Human Development on this topic that is very helpful. Click
For some unknown reason, we are suddenly receiving a lot of comments on our March 2010 posting on Endometriosis. Maybe it is because endometriosis is one of the most common gynecological diseases, affecting more that 5.5 million women in North America alone. There is a comprehensive fact sheet available from the National Institute of Child Health and Human Development on this topic that is very helpful. Click  A study by researchers at the National Institutes of Health (NIH) and the University of Oxford supports the widespread belief that stress may reduce a woman's chance of becoming pregnant. The study is the first of its kind to document, among women without a history of fertility problems, an association between high levels of a substance that is indicative of stress and a reduced chance of becoming pregnant.
A study by researchers at the National Institutes of Health (NIH) and the University of Oxford supports the widespread belief that stress may reduce a woman's chance of becoming pregnant. The study is the first of its kind to document, among women without a history of fertility problems, an association between high levels of a substance that is indicative of stress and a reduced chance of becoming pregnant.