 Surfacing research proves the Sub-Saharan African traditions of Female Genital Mutilation and Female Genital Cutting (FGM/FGC) lead to long-term health consequences. Such health problems are found to impact the delivery and health of newborns. Researchers and anthropologists from the Autonomus University of Barcelona collected data from 588 females in The Gambia. Data were carefully gathered through questionnaires and physical examinations of the female patients, and analyzed with 95% confidence intervals. The results showed that 75.6% of the women had undergone FGM or FGC, and these women had a significantly higher prevalence of health problems including dysmenorrhea, vulvar or vaginal pain, fibrosis, keloid, synechia, and sexual dysfunction. Furthermore, research showed these women were four times more likely to experience delivery complications such as perineal tear, obstructed labor, episiotomy, cesarean-necessitated delivery, and stillbirth.
Surfacing research proves the Sub-Saharan African traditions of Female Genital Mutilation and Female Genital Cutting (FGM/FGC) lead to long-term health consequences. Such health problems are found to impact the delivery and health of newborns. Researchers and anthropologists from the Autonomus University of Barcelona collected data from 588 females in The Gambia. Data were carefully gathered through questionnaires and physical examinations of the female patients, and analyzed with 95% confidence intervals. The results showed that 75.6% of the women had undergone FGM or FGC, and these women had a significantly higher prevalence of health problems including dysmenorrhea, vulvar or vaginal pain, fibrosis, keloid, synechia, and sexual dysfunction. Furthermore, research showed these women were four times more likely to experience delivery complications such as perineal tear, obstructed labor, episiotomy, cesarean-necessitated delivery, and stillbirth.
The Foundation for Research on Women’s Health reported that seven of The Gambia’s nine ethnic groups practice FGM or FGC on girls between the ages of 10 and 15. Female Genital Mutilation and Cutting occurs in four types. Type I is a partial clitoridectomy, Type II is a full removal of the clitoris, Type III is a partial or full excision of the external genitalia, and Type IV is vaginal sealing. While FGM and FGC are not common in many parts of the world, The Gambia sees these practices as rooted in customs and traditions dependent upon ethnic, religious, and cultural foundations. Culturally, these practices are seen as “rites of passage” into womanhood, and guarantee a woman’s sexual purity, as pleasure is removed from the woman’s body.
Alternatively, FGM and FGC have been internationally recognized as violations of women’s rights and cruel discriminations against women. Furthermore, since these practices are almost always carried out on minors, sometimes without parental consent, issues of children’s rights also come into play. The World Health Organization characterized these practices as violating “a person’s rights to health, security, and physical integrity” as well as “the right to be free from torture and cruel, inhuman or degrading treatment” especially when these practices frequently lead to death or long-term health problems.
While it is difficult to impose regulations on cultural traditions so foreign to the Western world, it is important to document the surfacing research that points to the long-term hazards that accompany these practices. The next steps should be educational outreaches informing the women of The Gambia of the dangers involved with FGM and FGC. This way, they may best make decisions to protect their reproductive health while preserving and respecting their cultural identity.
Sources: Dovepress, The UN Refugee Agency, and The World Health Organization

 The pro-life v. pro-choice debate continued on the House floor yesterday as party representatives grappled with sustaining women’s reproductive rights in a surfacing abortion bill. On Tuesday, the House of Representatives approved a bill banning a woman’s right to pursue an abortion after 22 weeks of pregnancy, subtracting two weeks off the current cut-off of abortions at 24 weeks in utero. The majority-Republican party passed this bill shaving off the extra two weeks based off the medically disputed theory that a fetus is capable of feeling pain 20 weeks after conception (which is equivalent to 22 weeks of pregnancy). Democrats in the House and the White House fought against the bill, saying the legislation is an “assault on a woman’s right to choose” and is an attempt to undermine the precedent set in the 1973
The pro-life v. pro-choice debate continued on the House floor yesterday as party representatives grappled with sustaining women’s reproductive rights in a surfacing abortion bill. On Tuesday, the House of Representatives approved a bill banning a woman’s right to pursue an abortion after 22 weeks of pregnancy, subtracting two weeks off the current cut-off of abortions at 24 weeks in utero. The majority-Republican party passed this bill shaving off the extra two weeks based off the medically disputed theory that a fetus is capable of feeling pain 20 weeks after conception (which is equivalent to 22 weeks of pregnancy). Democrats in the House and the White House fought against the bill, saying the legislation is an “assault on a woman’s right to choose” and is an attempt to undermine the precedent set in the 1973  Policy changes are necessary to decrease the death rate of pregnant women in developing countries. Research, according to Dr. Stacie E. Geller, does not end once scientists publish. The true battle is implementing that research to affect global change. Dr. Stacie E. Geller, Director of the Center for Research on Women and Gender at the University of Illinois at Chicago College of Medicine, puts research into practice by providing safe, affordable medication to pregnant women in developing countries. Dr. Geller spoke last week at a forum held at Northwestern University's Feinberg School of Medicine and presented her research on Postpartum Hemorrhaging (PPH) and its dangers to women in developing countries.
Policy changes are necessary to decrease the death rate of pregnant women in developing countries. Research, according to Dr. Stacie E. Geller, does not end once scientists publish. The true battle is implementing that research to affect global change. Dr. Stacie E. Geller, Director of the Center for Research on Women and Gender at the University of Illinois at Chicago College of Medicine, puts research into practice by providing safe, affordable medication to pregnant women in developing countries. Dr. Geller spoke last week at a forum held at Northwestern University's Feinberg School of Medicine and presented her research on Postpartum Hemorrhaging (PPH) and its dangers to women in developing countries. Think men and women receive equal care after traumas? Think again. A recent study found that women are less likely than men to receive trauma treatment after severe injuries. Dr. Andrea Hill of the Sunnybrook Health Sciences Centre and the University of Toronto’s research on gender-based inequalities found that, across all age groups, 20-30% fewer women are cared for after traumas. The study and analysis were conducted by observing 99,000 adult patients throughout Canada. After controlling for demographic and socioeconomic factors, Hill and her colleagues were shocked at such disproportions between male and female patient care. Hill affirms that “gender-based disparities in access to health care services in general have been recognized for some time,” and she calls for further research into the underlying factors involved in these gender gaps.
Think men and women receive equal care after traumas? Think again. A recent study found that women are less likely than men to receive trauma treatment after severe injuries. Dr. Andrea Hill of the Sunnybrook Health Sciences Centre and the University of Toronto’s research on gender-based inequalities found that, across all age groups, 20-30% fewer women are cared for after traumas. The study and analysis were conducted by observing 99,000 adult patients throughout Canada. After controlling for demographic and socioeconomic factors, Hill and her colleagues were shocked at such disproportions between male and female patient care. Hill affirms that “gender-based disparities in access to health care services in general have been recognized for some time,” and she calls for further research into the underlying factors involved in these gender gaps. A new report by the Institute of Medicine issued on Sept. 23, concludes that there has been some progress in women's health over the past two decades especially in lessening the burden of disease and reduced deaths among women in the areas of cardiovascular disease, breast cancer and cervical cancer, specifically. The effort has yielded less but still significant progress in reducing the effects of depresssion, HIV/AIDS, and osteoporosis in women. However, the report also identifies several areas that are important to women that have seen little progress, namely, unintended pregnancy, autoimmune disease, alcohol and drug addiction, lung cancer, and dementia.
A new report by the Institute of Medicine issued on Sept. 23, concludes that there has been some progress in women's health over the past two decades especially in lessening the burden of disease and reduced deaths among women in the areas of cardiovascular disease, breast cancer and cervical cancer, specifically. The effort has yielded less but still significant progress in reducing the effects of depresssion, HIV/AIDS, and osteoporosis in women. However, the report also identifies several areas that are important to women that have seen little progress, namely, unintended pregnancy, autoimmune disease, alcohol and drug addiction, lung cancer, and dementia. Older men may be at risk of developing mild cognitive impairment (MCI), often a precursor to Alzheimer’s disease, earlier in life than older women, according to a study appearing today in Neurology. The study raises the question of whether there may be a gender difference in the development and progression of MCI.
Older men may be at risk of developing mild cognitive impairment (MCI), often a precursor to Alzheimer’s disease, earlier in life than older women, according to a study appearing today in Neurology. The study raises the question of whether there may be a gender difference in the development and progression of MCI.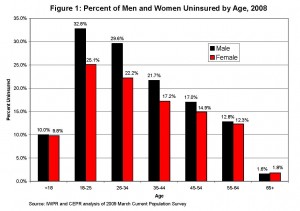
 Several Northwestern researchers, including our own
Several Northwestern researchers, including our own 

