 No, you did not open the wrong page. Yes, this blog is posted by the Institute for Women's Health Research at Northwestern. As an advocate for better sex and gender based research, we support all avenues that increase our knowledge about sex differences and that includes a better understanding of hormone changes in women AND MEN.
No, you did not open the wrong page. Yes, this blog is posted by the Institute for Women's Health Research at Northwestern. As an advocate for better sex and gender based research, we support all avenues that increase our knowledge about sex differences and that includes a better understanding of hormone changes in women AND MEN.
Furthermore, women are generally the source of health information for their families and that includes their male partners! So, women and men, read on!
 Low testosterone levels to blame for low libido, fatigue and weight gain
Low testosterone levels to blame for low libido, fatigue and weight gain
While most frequently associated with women’s health, age-related hormone changes, often dubbed menopause, can occur in men as well, causing symptoms of fatigue, mood swings, decreased desire for sex, hair loss, lack of concentration and weight gain. Experts estimate that more than 5 million men are affected, yet worry the number may be considerably higher since symptoms are frequently ignored. Male hypogonadism, as it’s referred to in the medical community, occurs when the testicles do not produce enough testosterone, the hormone that plays a key role in masculine growth and development. When hormone levels drop, men can experience significant mental and physical changes.
“This is a highly prevalent disorder,” said Robert Brannigan, MD, urologist at Northwestern Memorial Hospital. “Unfortunately, we estimate that 95 percent of cases are undiagnosed and therefore untreated. When ignored, symptoms can seriously disrupt one’s quality of life.”
Brannigan explains hormone variations are a normal aspect of getting older. “In females, ovulation comes to an end and hormone production declines in a relatively quick period of time, whereas men experience hormone shifts more slowly, with testosterone levels dropping around one percent each year beginning in a man’s late thirties,” adds Brannigan. He goes on to explain that by age seventy, the reduction in a male’s testosterone level could be as high as fifty percent or more compared to baseline levels, but notes that aging men are not the only ones at risk. A number of genetic causes can impact males from birth and are usually diagnosed with failure to progress normally through puberty during the teenage years.
Treatment options for male hypogonadism include hormone replacement therapy (HRT) via absorbable pellet implants, topical gels, patches, and injections. Through HRT, doctors can restore sexual function and muscle strength. In addition, men often experience an increase in energy and an improved overall sense of well-being.
“We are seeing more men affected by male hypogonadism than we saw ten years ago,” said Brannigan. “However, many men continue to suffer in silence due to a lack of awareness surrounding the disorder. Because male hypogonadism can significantly impact the quality of one’s life, it’s important that men pay attention to their body and openly discuss symptoms with their physician in order to prevent overlooking the cause and avoid missing an opportunity for appropriate therapy.”
Although research to determine the exact association continues, doctors also warn that male hypogonadism has been linked to chronic medical conditions such as high cholesterol, diabetes and cardiovascular disease. It’s also closely associated with infertility.
“This disorder is not something that should be ignored,” said Brannigan, who is working to educate patients and physicians about the symptoms and treatments available in order to ensure therapies are made available to men in need.
Male hypogonadism is most commonly diagnosed through a simple blood test. Brannigan notes hormone replacement therapy is not appropriate for all patients especially those with history of prostate and breast cancer and men trying to conceive. He suggests consulting your doctor if you are experiencing symptoms.
 A recent Food and Drug Administration (FDA) MedWatch Safety Alert warns women to make sure children and pets do not come into contact with Evamist that they have sprayed on their skin. Evamist is a transdermal spray containing estradiol, a form of estrogen. It is sprayed inside of the forearm between the elbow and wrist to reduce hot flashes during menopause. Each squirt of spray delivers 90 mcL which contains 1.53 mg of estradiol and is FDA approved for this use.
A recent Food and Drug Administration (FDA) MedWatch Safety Alert warns women to make sure children and pets do not come into contact with Evamist that they have sprayed on their skin. Evamist is a transdermal spray containing estradiol, a form of estrogen. It is sprayed inside of the forearm between the elbow and wrist to reduce hot flashes during menopause. Each squirt of spray delivers 90 mcL which contains 1.53 mg of estradiol and is FDA approved for this use.
 No, you did not open the wrong page. Yes, this blog is posted by the
No, you did not open the wrong page. Yes, this blog is posted by the  Low testosterone levels to blame for low libido, fatigue and weight gain
Low testosterone levels to blame for low libido, fatigue and weight gain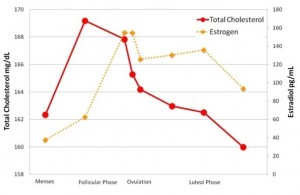 Women's cholesterol levels vary with phase of menstrual cycle
Women's cholesterol levels vary with phase of menstrual cycle