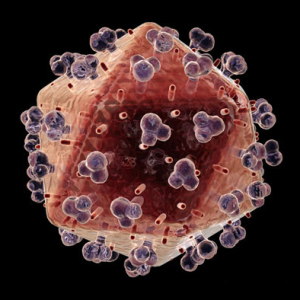
It’s often said that the HIV/AIDS epidemic has a woman’s face. The proportion of women infected with HIV has been on the rise for a decade; in sub-Saharan Africa, women constitute 60 percent of people living with the disease. While preventative drugs exist, they have often proven ineffective, especially in light of financial and cultural barriers in developing nations.
It’s often said that the HIV/AIDS epidemic has a woman’s face. The proportion of women infected with HIV has been on the rise for a decade; in sub-Saharan Africa, women constitute 60 percent of people living with the disease. While preventative drugs exist, they have often proven ineffective, especially in light of financial and cultural barriers in developing nations.
A new intravaginal ring filled with an anti-retroviral drug could help. Developed with support from the National Institute of Allergy and Infectious Diseases by Northwestern University visiting associate professor Patrick Kiser, PhD, the ring is easy to use, long lasting and recently demonstrated a 100 percent success rate protecting primates from the simian human immunodeficiency virus (SHIV). The device will soon undergo its first test in humans.
“After 10 years of work, we have created an intravaginal ring that can prevent against multiple HIV exposures over an extended period of time, with consistent prevention levels throughout the menstrual cycle,” said Kiser, an expert in intravaginal drug delivery who joined Northwestern from the University of Utah, where the research was conducted.
The research was published Sept. 16 in the Proceedings of the National Academy of Sciences (PNAS).
Previous studies have demonstrated that antiviral drugs can prevent HIV infection, but existing methods for delivering the drug fall short. Pills must be taken daily and require high doses; vaginal gels that must be applied prior to each sex act are inconvenient, yielding poor usage rates. The new ring is easily inserted and stays in place for 30 days. And because the drug is delivered at the site of transmission, the ring -- known as a TDF-IVR (tenofovir disoproxil fumarate intravaginal ring) -- utilizes a smaller dose than pills.
The upcoming clinical trial, to be conducted in November at Albert Einstein College of Medicine in New York, will evaluate Kiser’s ring in 30 women over 14 days. The trial will assess the ring’s safety and measure how much of the drug is released and the properties of the ring after use.
The paper is titled “Intravaginal Ring Eluting Tenofovir Disoproxil Fumarate Completely Protects Macaques from Multiple Vaginal Simian-HIV Challenges.”
Source: Megan Fellman on Oct 03, 2013

 Nearly 25% of those infected with HIV/AIDS in the United States are female. In recognition of National Women and Girls HIV/AIDS Awareness Day on March 10, take a few minutes to learn basic facts about prevention, testing, and issues specific to women. These resources will help:
Nearly 25% of those infected with HIV/AIDS in the United States are female. In recognition of National Women and Girls HIV/AIDS Awareness Day on March 10, take a few minutes to learn basic facts about prevention, testing, and issues specific to women. These resources will help: It's generally known that women's genital tissue is more susceptible to the HIV virus that causes AIDS. Researcher are studying the various types of epithelial cells in the reproductive tract and the possible protective role of mucus to try to determine what makes women more vulnerable to the spread of this virus. A new study supported by the National Institute of Child Health and Human Development (NCHID) at the NIH found that an immune system protein normally found in semen may enhance the spread of HIV to tissue from the uterine cervix. The protein interleukin 7 (IL-7) belongs to a family of proteins that regulates the immune response and is present normally in semen but at even higher levels in the semen in men with HIV.
It's generally known that women's genital tissue is more susceptible to the HIV virus that causes AIDS. Researcher are studying the various types of epithelial cells in the reproductive tract and the possible protective role of mucus to try to determine what makes women more vulnerable to the spread of this virus. A new study supported by the National Institute of Child Health and Human Development (NCHID) at the NIH found that an immune system protein normally found in semen may enhance the spread of HIV to tissue from the uterine cervix. The protein interleukin 7 (IL-7) belongs to a family of proteins that regulates the immune response and is present normally in semen but at even higher levels in the semen in men with HIV. On Tuesday, December 18th the
On Tuesday, December 18th the  Despite stable rates of HIV diagnosis in older populations, the rate of HIV diagnoses from 2006 to 2009 increased in teens 15-19 and youth 20-24 years of age, and was highest in the 20-24 year-old age group. Undiagnosed HIV cases are also thought to be highest among young people. The U.S. Centers for Disease Control and Prevention (CDC) estimates more than half of all undiagnosed HIV infections are youth ages 13 – 24.3.
Despite stable rates of HIV diagnosis in older populations, the rate of HIV diagnoses from 2006 to 2009 increased in teens 15-19 and youth 20-24 years of age, and was highest in the 20-24 year-old age group. Undiagnosed HIV cases are also thought to be highest among young people. The U.S. Centers for Disease Control and Prevention (CDC) estimates more than half of all undiagnosed HIV infections are youth ages 13 – 24.3. Pregnant women who are unaware that they have HIV miss the chance for drug treatment that can benefit not only their own health, but could also prevent them from transmitting the virus to their infants. When HIV is not diagnosed until women go into labor, their infants are usually treated soon after birth with the anti HIV drug zidovudine (ZDV), to prevent the infants from becoming infected with the virus.
Pregnant women who are unaware that they have HIV miss the chance for drug treatment that can benefit not only their own health, but could also prevent them from transmitting the virus to their infants. When HIV is not diagnosed until women go into labor, their infants are usually treated soon after birth with the anti HIV drug zidovudine (ZDV), to prevent the infants from becoming infected with the virus. December 1 is World AIDS Day and the
December 1 is World AIDS Day and the  The health of pregnant women can say a lot about a region. It can indicate the accessibility and affordability of health care, as well as how much recognition maternal health receives in the region. A healthy pregnancy results in healthier children and decreased risk for maternal death. Conversely, measuring maternal mortality rates can also indicate the level of health resources within a country
The health of pregnant women can say a lot about a region. It can indicate the accessibility and affordability of health care, as well as how much recognition maternal health receives in the region. A healthy pregnancy results in healthier children and decreased risk for maternal death. Conversely, measuring maternal mortality rates can also indicate the level of health resources within a country