Benefits shown in middle-aged and elderly women
 Middle-aged and elderly Swedish women who regularly ate a small amount of chocolate had lower risks of heart failure risks, in a study reported in Circulation: Heart Failure, a journal of the American Heart Association. The nine-year study, conducted among 31,823 middle-aged and elderly Swedish women, looked at the relationship of the amount of high-quality chocolate the women ate, compared to their risk for heart failure. The quality of chocolate consumed by the women had a higher density cocoa content somewhat like dark chocolate by American standards. In this study, researchers found:
Middle-aged and elderly Swedish women who regularly ate a small amount of chocolate had lower risks of heart failure risks, in a study reported in Circulation: Heart Failure, a journal of the American Heart Association. The nine-year study, conducted among 31,823 middle-aged and elderly Swedish women, looked at the relationship of the amount of high-quality chocolate the women ate, compared to their risk for heart failure. The quality of chocolate consumed by the women had a higher density cocoa content somewhat like dark chocolate by American standards. In this study, researchers found:
- Women who ate an average of one to two servings of the high-quality chocolate per week had a 32 percent lower risk of developing heart failure.
- Those who had one to three servings per month had a 26 percent lower risk.
- Those who consumed at least one serving daily or more didn’t appear to benefit from a protective effect against heart failure.
The lack of a protective effect among women eating chocolate every day is probably due to the additional calories gained from eating chocolate instead of more nutritious foods, said Murrray Mittleman, M.D., Dr.P.H., lead researcher of the study. “You can’t ignore that chocolate is a relatively calorie-dense food and large amounts of habitual consumption is going to raise your risks for weight gain,” said Mittleman, director of the Cardiovascular Epidemiology Research Unit at Harvard Medical School’s Beth Israel Deaconess Medical Center in Boston. “But if you’re going to have a treat, dark chocolate is probably a good choice, as long as it’s in moderation.”
High concentration of compounds called “flavonoids” in chocolate may lower blood pressure, among other benefits, according to mostly short-term studies. However, this is the first study to show long-term outcomes related specifically to heart failure, which can result from ongoing untreated high blood pressure. In the observational study, researchers analyzed self-reported food-frequency questionnaire responses from participants 48-to-83-years-old in the Swedish Mammography Cohort. Combining the results with data from national Swedish hospitalization and death registries between 1998 through 2006, the researchers used multiple forms of statistical modeling to reach their conclusions on heart failure and chocolate consumption.
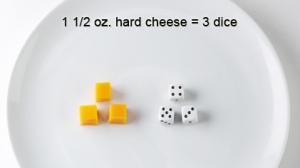
Mittleman said differences in chocolate quality affect the study’s implications for Americans. Higher cocoa content is associated with greater heart benefits. In Sweden, even milk chocolate has a higher cocoa concentration than dark chocolate sold in the United States. Although 90 percent of all chocolate eaten across Sweden during the study period was milk chocolate, it contained about 30 percent cocoa solids. U.S. standards only require 15 percent cocoa solids to qualify as dark chocolate. So, by comparison, American chocolate may have fewer heart benefits and more calories and fat per equivalent amounts of cocoa content compared to the chocolate eaten by the Swedish women in the study. Also, the average serving size for Swedish women in the study ranged from 19 grams among those 62 and older, to 30 grams among those 61 and younger. In contrast, the standard American portion size is 20 grams.
“Those tempted to use these data as their rationale for eating large amounts of chocolate or engaging in more frequent chocolate consumption are not interpreting this study appropriately,” said Linda Van Horn, Ph.D., R.D., immediate past chair of the American Heart Association Nutrition Committee and professor in the Department of Preventive Medicine at Northwestern University’s Feinberg School of Medicine in Chicago. “This is not an ‘eat all you want’ take-home message, rather it’s that eating a little dark chocolate can be healthful, as long as other adverse behaviors do not occur, such as weight gain or excessive intake of non-nutrient dense ‘empty’ calories.”
Heart failure occurs among about 1 percent of Americans over age 65. A condition in which the heart can’t pump enough blood to the rest of the body, heart failure rates are increasing as our aging population grows.“Anything that helps to decrease heart failure is an important issue worth examining,” Mittleman said.
Co-authors are Elizabeth Mostofsky, M.P.H.; Emily Levitan, Sc.D.; and Alicja Wolk, Dr.Med.Sci. Author disclosures and funding support are on the manuscript.
Source: Press release prepared by the American Heart Association


 In July, a commentary in the journal
In July, a commentary in the journal  I just received a FDA email about the safety of color additives in food. What caught my eye was the subheading: "Without color additives, colas wouldn't be brown, margarine wouldn't be yellow and mint ice cream wouldn't be green." I wonder if colorless food could help reduce the obesity epidemic!!! Seriously, to read the article, click
I just received a FDA email about the safety of color additives in food. What caught my eye was the subheading: "Without color additives, colas wouldn't be brown, margarine wouldn't be yellow and mint ice cream wouldn't be green." I wonder if colorless food could help reduce the obesity epidemic!!! Seriously, to read the article, click 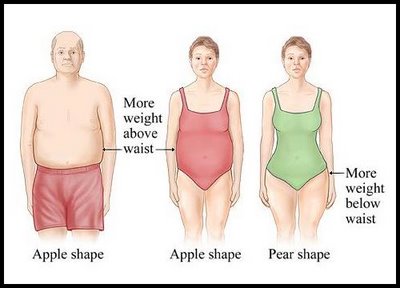 CHICAGO --- The more an older woman weighs, the worse her memory, according to new research from Northwestern Medicine. The effect is more pronounced in women who carry excess weight around their hips, known as pear shapes, than women who carry it around their waists, called apple shapes. The study of 8,745 cognitively normal, post-menopausal women ages 65 to 79 from the Women's Health Initiative hormone trials is the first in the United States to link obesity to poorer memory and brain function in women and to identify the body-shape connection.
CHICAGO --- The more an older woman weighs, the worse her memory, according to new research from Northwestern Medicine. The effect is more pronounced in women who carry excess weight around their hips, known as pear shapes, than women who carry it around their waists, called apple shapes. The study of 8,745 cognitively normal, post-menopausal women ages 65 to 79 from the Women's Health Initiative hormone trials is the first in the United States to link obesity to poorer memory and brain function in women and to identify the body-shape connection. The Agency for Healthcare Research and Quality issued its 2009 National Healthcare Quality Report and National Healthcare Disparities Report on April 13. The 2009 reports include a new section on lifestyle modifications because preventing or reducing obesity is a crucial national goal. The reports found:
The Agency for Healthcare Research and Quality issued its 2009 National Healthcare Quality Report and National Healthcare Disparities Report on April 13. The 2009 reports include a new section on lifestyle modifications because preventing or reducing obesity is a crucial national goal. The reports found: