 Last week Health Canada released an official warning on the association of increased risk of bone fracture with the frequent use of Proton-Pump Inhibitor (PPI) medications, used to treat symptoms of acid reflux and gastroesophegeal reflux disease (GERD). While an important step, this warning, like the U.S. FDA’s before it, does not go far enough in ensuring that the public is aware of the immense risks posed by continuous dosages of PPI pills, particularly to women.
Last week Health Canada released an official warning on the association of increased risk of bone fracture with the frequent use of Proton-Pump Inhibitor (PPI) medications, used to treat symptoms of acid reflux and gastroesophegeal reflux disease (GERD). While an important step, this warning, like the U.S. FDA’s before it, does not go far enough in ensuring that the public is aware of the immense risks posed by continuous dosages of PPI pills, particularly to women.
According to the alert, “several scientific studies suggest that PPI therapy may be associated with a small increased risk for fractures of the hip, wrist, or spine related to osteoporosis, a disease resulting in the weakening of bones.” They added that “the risk of fracture was higher in patients who received multiple daily doses of PPIs and therapy for a year or longer. Additional risk factors for osteoporosis, such as age, gender and the presence of other health conditions, may also contribute to the increased risk of fractures.”[1] Though the alert mentions that gender could also contribute to the increased risk, what the alert fails to mention is that women face the greatest risks when taking these pills.
Last year, a team of researchers from Harvard Medical School and Boston General Hospital in a study focusing on over 80,000 post-menopausal women, found that among those who had taken PPI pills 3-4 times per week over a two-year period had an increased risk of hip-fracture of 35%. For current and former smokers, the increase was as high as 50%.[2] A common theory for the cause of this increase is the fact that the pills inhibit the body’s ability to intake calcium, an essential element for maintaining strong bones.
These aren’t the only problems associated with PPI pills, however. Though the warning labels on nearly all PPI’s, including those sold by major brands like Prilosec®, Nexium®, and Prevacid®, state that the pills should be taken for a maximum of fourteen days annually, many patients continue with daily therapy for years. These medications,, which treat short-term symptoms of acid reflux by blocking the stomach’s natural production of acid, have serious negative side-effects. According to the FDA, prolonged dosages of PPI pills can lead to an increase in risk of pneumonia, heart arrhythmia, and Clostridium difficile–associated diarrhea.[3] Worse, according to a study by Dr. Blair Jobe at the University of Pittsburg, those taking PPI pills regularly to treat mild symptoms were 60% more likely to suffer from Barrett’s Esophagus, which often leads to esophageal cancer.[4]
In response to Health Canada’s warning, Dr. William Dengler, Medical Director of RefluxMD, issued this response: “In light of a recent warning by the Canadian federal government, PPI users and their physicians should carefully consider the long-term side effects when using these drugs. These same side effects are responsible for the U.S. FDA placing this class of drugs on their "watch list." With multiple governments warning patients that the side effects for acid reflux medications are troublesome, the media should play a larger role in combatting the over-saturation of television marketing for the drugs.”[5] More importantly, however, consumers, particularly women, should pay careful attention to the risks associated with PPI pills before starting treatment, as well as consider natural alternatives that could help to treat long-term causes of acid-reflux, rather than short-term symptoms.
Guest Blogger: Alexander Michael Jakubowski, Northwestern Undergraduate Student
 In May, 2013, the American College of Gastroenterology has published new guidelines for diagnosing and managing gastroesophageal reflux disease (GERD). Dr. Lauren B. Gerson from Stanford University School of Medicine, California, a member of the guidelines panel, highlighted six areas where the guidelines changed since the 2005 version:
In May, 2013, the American College of Gastroenterology has published new guidelines for diagnosing and managing gastroesophageal reflux disease (GERD). Dr. Lauren B. Gerson from Stanford University School of Medicine, California, a member of the guidelines panel, highlighted six areas where the guidelines changed since the 2005 version: Most of us get heartburn from time to time. It may come as a burning sensation in the chest, or a bitter taste in the back of the throat. Heartburn is one word people use to describe reflux. It happens when stomach contents come back upwards. Reflux is sometimes painless: You may have trouble swallowing or get a dry cough, perhaps some wheezing.
Most of us get heartburn from time to time. It may come as a burning sensation in the chest, or a bitter taste in the back of the throat. Heartburn is one word people use to describe reflux. It happens when stomach contents come back upwards. Reflux is sometimes painless: You may have trouble swallowing or get a dry cough, perhaps some wheezing.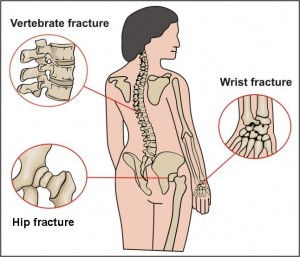 A recent publication from the National Osteoporosis Foundation reported that many women with postmenopausal osteoporosis underestimate their risk for fractures. This is particularly alarming when it is coupled with new information released from the Food and Drug Administration (FDA) that found potential increased risk of fracture of the hip, wrist and spine if you take certain drugs for heartburn, acid reflux, or ulcers.
A recent publication from the National Osteoporosis Foundation reported that many women with postmenopausal osteoporosis underestimate their risk for fractures. This is particularly alarming when it is coupled with new information released from the Food and Drug Administration (FDA) that found potential increased risk of fracture of the hip, wrist and spine if you take certain drugs for heartburn, acid reflux, or ulcers.