A recent study published in Environmental Science & Technology tied a group of chemicals called benzophenones to an increased risk of endometriosis. The study measured the amount of benzophenones in the urine of 600 women who were tested for endometriosis. One particular benzophenone, benzophenone-1, showed a significant association with the condition. Compared to women with low levels, women who had the highest concentration of this chemical in their urine showed a 65% greater chance of having the condition. In a separate study, the CDC found benzophenones in the urine of 97% of people tested. With one in ten women having endometriosis, benzophenone-1 may be the cause.
A recent study published in Environmental Science & Technology tied a group of chemicals called benzophenones to an increased risk of endometriosis. The study measured the amount of benzophenones in the urine of 600 women who were tested for endometriosis. One particular benzophenone, benzophenone-1, showed a significant association with the condition. Compared to women with low levels, women who had the highest concentration of this chemical in their urine showed a 65% greater chance of having the condition. In a separate study, the CDC found benzophenones in the urine of 97% of people tested. With one in ten women having endometriosis, benzophenone-1 may be the cause.
Benzophenones protect against UV light. In small quantities, like nail polish, it stabilizes compounds that are stored in clear containers. When used in a higher concentration, such as on the skin, it becomes a good sunscreen. Benzophenone-1 in particular can be produced from oxybenzone (or benzophenone-3), a chemical penetration enhancer found in sunscreen, when the body breaks it down.
Interestingly, the CDC also linked benzophenone-3 to many other health issues such as allergies, hormone disruption, cell damage and low birth weight in female babies. Among sunscreen, the chemical can also be found in facial cleansers/treatments, lip balm, lipstick, anti-aging creams, conditioners and perfume.
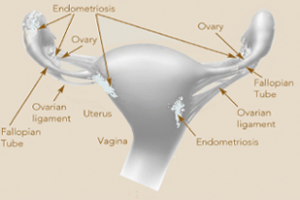
Endometriosis, a gynecological condition, occurs when tissue from the uterus grows outside of the uterus instead of inside it. The tissue can start to grow in other places such as into the abdomen, outside the ovaries and around the fallopian tubes. It thickens and sheds simultaneously with the tissue inside of the uterus during the menstrual cycle. The condition causes pain, irregular bleeding, scarring and can cause infertility.
The group of chemicals mimics estrogen, and while researchers cannot definitively pinpoint the cause of the condition, they do know that estrogen enhances the condition. Treatment usually involves medications to lower the amount of estrogen in the body.
The Personal Care Products Council, which represents cosmetics manufacturers, said that the study was weak and unconvincing and should not be a deterrent from sunscreen or safe-sun practices. The group says the study did not ask participants if (or how much) sunscreen they wore, therefore they couldn’t attribute the results directly to sunscreen.
Conversely, women in California had higher concentrations of the chemical when tested during the summer, suggesting that sunscreen is the culprit, according to Sonya Lunder, MPH of the Environmental Working Group. The CDC found similar results in light-skinned women who were tested, further confirming Lunder’s theory.
Many of the findings seem conflicting. The best advice may be to find a sunscreen without the chemical, such as one that is mineral-based, containing zinc oxide or titanium dioxide. These varieties block the sun naturally, so you can protect yourself against both the condition and the harmful UV rays.
Sunscreens without Oxybenzone:
Natural Sun SPF 30 Sunscreen for Active Lifestyles
Oat Protein Sunscreen SPF 30 by Kiss My Face
Read more about the topic here or here.

 Researchers have identified a key step in the establishment of a pregnancy. The discovery may shed light on fertility disorders and diseases of the uterus, including endometrial cancer. At the start of each menstrual cycle, levels of the hormone estrogen begin to rise, which causes the uterine lining to grow and thicken. When the ovary releases an egg, levels of another hormone, progesterone, increase. Higher progesterone levels put the brakes on the estrogen-driven growth of the uterine lining, allowing the lining to mature and egg implantation to take place. Because of this function, progesterone is sometimes given to women to treat infertility and prevent premature birth. However, it carries some unpleasant side effects. A greater understanding of how progesterone works could lead to better treatments. It could also shed light on disorders such as endometrial cancer and endometriosis, which is marked by uncontrolled growth of the uterine lining. To clarify how progesterone stops the growth of the uterine lining, the study's first author, Dr. Quanxi Li of the University of Illinois at Urbana-Champaign, led a group of researchers from several institutions. Their findings were published in the February 28, 2011, issue of Science. The team focused on the role of a protein called Hand2 in halting the growth of the uterine lining. They had previously found that blocking the progesterone receptor decreased Hand2 expression in uterine cells, indicating a link between Hand2 and progesterone.In their new study, the team genetically engineered mice to lack Hand2 in the uterus, and then gave them progesterone. They then stimulated uterine lining growth with estrogen. In normal mice, progesterone prevents the uterine lining from growing. In the mice without Hand2, however, the lining grew in spite of the progesterone treatment. The scientists found that uterine cells beneath the lining express Hand2 during egg implantation. Further experiments revealed that estrogen stimulates the production of molecules called growth factors, which cause the uterine lining to grow. High levels of Hand2, brought on by progesterone, stop the production of these growth factors. Therefore, the uterine lining stops growing, allowing egg implantation. The discovery of Hand2's role in halting growth of the uterine lining may spur development of treatments for diseases like endometriosis and endometrial cancer. "This information helps us understand how the interplay of hormones prepares the uterus to host and support the embryo as it grows," says Dr. Milan Bagchi, a senior author of the study. "Our next priority will be to examine whether Hand2 plays a critical role in the human uterus as well." Related Links:
Researchers have identified a key step in the establishment of a pregnancy. The discovery may shed light on fertility disorders and diseases of the uterus, including endometrial cancer. At the start of each menstrual cycle, levels of the hormone estrogen begin to rise, which causes the uterine lining to grow and thicken. When the ovary releases an egg, levels of another hormone, progesterone, increase. Higher progesterone levels put the brakes on the estrogen-driven growth of the uterine lining, allowing the lining to mature and egg implantation to take place. Because of this function, progesterone is sometimes given to women to treat infertility and prevent premature birth. However, it carries some unpleasant side effects. A greater understanding of how progesterone works could lead to better treatments. It could also shed light on disorders such as endometrial cancer and endometriosis, which is marked by uncontrolled growth of the uterine lining. To clarify how progesterone stops the growth of the uterine lining, the study's first author, Dr. Quanxi Li of the University of Illinois at Urbana-Champaign, led a group of researchers from several institutions. Their findings were published in the February 28, 2011, issue of Science. The team focused on the role of a protein called Hand2 in halting the growth of the uterine lining. They had previously found that blocking the progesterone receptor decreased Hand2 expression in uterine cells, indicating a link between Hand2 and progesterone.In their new study, the team genetically engineered mice to lack Hand2 in the uterus, and then gave them progesterone. They then stimulated uterine lining growth with estrogen. In normal mice, progesterone prevents the uterine lining from growing. In the mice without Hand2, however, the lining grew in spite of the progesterone treatment. The scientists found that uterine cells beneath the lining express Hand2 during egg implantation. Further experiments revealed that estrogen stimulates the production of molecules called growth factors, which cause the uterine lining to grow. High levels of Hand2, brought on by progesterone, stop the production of these growth factors. Therefore, the uterine lining stops growing, allowing egg implantation. The discovery of Hand2's role in halting growth of the uterine lining may spur development of treatments for diseases like endometriosis and endometrial cancer. "This information helps us understand how the interplay of hormones prepares the uterus to host and support the embryo as it grows," says Dr. Milan Bagchi, a senior author of the study. "Our next priority will be to examine whether Hand2 plays a critical role in the human uterus as well." Related Links:  For some unknown reason, we are suddenly receiving a lot of comments on our March 2010 posting on Endometriosis. Maybe it is because endometriosis is one of the most common gynecological diseases, affecting more that 5.5 million women in North America alone. There is a comprehensive fact sheet available from the National Institute of Child Health and Human Development on this topic that is very helpful. Click
For some unknown reason, we are suddenly receiving a lot of comments on our March 2010 posting on Endometriosis. Maybe it is because endometriosis is one of the most common gynecological diseases, affecting more that 5.5 million women in North America alone. There is a comprehensive fact sheet available from the National Institute of Child Health and Human Development on this topic that is very helpful. Click