 You may have heard the buzz this summer about the little pink flibanserin pill, an experimental drug that has been created to boost female libido. This pill, made by Sprout Pharmaceuticals, is the first drug that has claimed to boost female sexual desire and has sparked intense and emotional debates about whether or not the U.S. Food and Drug Administration (FDA) should approve it. The debate has garnered a lot of media attention and public response, all of which can be confusing and misleading depending on the source. We’re here to synthesize the information.
You may have heard the buzz this summer about the little pink flibanserin pill, an experimental drug that has been created to boost female libido. This pill, made by Sprout Pharmaceuticals, is the first drug that has claimed to boost female sexual desire and has sparked intense and emotional debates about whether or not the U.S. Food and Drug Administration (FDA) should approve it. The debate has garnered a lot of media attention and public response, all of which can be confusing and misleading depending on the source. We’re here to synthesize the information.
What is flibanserin?
Flibanserin is the pill that targets lost libido in pre-menopausal women by enhancing sexual desire and decreasing emotional distress. The experimental drug has often been referred to as “female Viagra.” This nickname, however, is misleading as the two drugs work in completely different ways. Viagra helps men get and keep an erection by increasing the blood flow to the penis. In contrast, flibanserin targets the brain, not the genitals.
Specifically, the drug shifts the balance of three key chemicals in the brain: dopamine, norepinephrine, and serotonin. Dopamine is a neurotransmitter that helps control the brain’s reward and pleasure centers and is increased by the drug to help increase interest in sex. Norepinephrine is a neurotransmitter that helps the brain control our attention and focus. The targeting and increase of these two chemicals is said to increase the “excitatory factors for sex.” The drug also decreases serotonin, which is known to decrease sex drive.
The Debates
Before this year, flibanserin has been rejected twice by the FDA. The first rejection occurred in 2010 over both concerns of the cited side effects, which included nausea, dizziness, and sleepiness as well as its limited effectiveness shown in clinical trials. Three years later in 2013, the drug was rejected again for continuing to show limited benefits to patients – the agency said that additional studies needed to be conducted to show that the benefit of the drug outweighed the risks.
At the beginning of June 2015, the drug was once again brought before the advisory committee of the FDA and the committee voted in favor of approving the pill as long as there are significant measures in place to make sure that women are aware of the risks and side effects. While the committee did vote in favor, the debate continues to grow about whether or not the FDA should follow the committee’s suggestion.
The first point is that the benefits of the drug are controversial. Clinical trials of flibanserin reported that women who took the drug had an average increase of 1.0 more satisfying sexual events per month than women who took a placebo. The effectiveness, therefore, is debated: some people say that one extra episode of satisfying sex per month is significant, while others say it is not enough of an increase to be deemed effective.
A second point of debate is regarding the side effects of the drug. Every drug has side effects and the listed ones for flibanserin include sleepiness, nausea, and dizziness. There are also reports of fainting and drowsiness, which has been shown to lead to a higher risk of accidents, and there are concerns about the potential increases risk for these side effects when the drug is combined with alcohol. Another area of concern that has been expressed is that it is unknown whether flibanserin interferes with SSRI antidepressants, such as Prozac, which boost serotonin levels in the brain.
One of the most pressing risks identified by people who are wary about the drug is the unknown long-term health risk. The clinical trials were too short to identify the possible long-term risks of taking the pill daily.
The other big debate surrounds the idea that the campaign for this drug is oversimplifying female sexuality and changing sexuality into a medical problem. According to Adriane Fugh-Berman, who studies drug companies at Georgetown University, this is seen as part of a larger trend in the United States of pharmaceutical companies “medicalizing the normal human experience” and turning “everything into a disease that needs a pill.” It is not uncommon for women to have symptoms of low libido and some argue that medication is not the answer for everyone. Low libido can be the symptom of many different issues to which flibanserin might not be the best solution, including fluctuating hormones, depression, fatigue, stress, interpersonal dynamics with a partner, and lack of foreplay, among other pharmacological, psychological, and physical issues. People on the other side of the debate argue that since women, unlike men, do not yet have a medication that addresses low sex drive, the approval of flibanserin is crucial for this scientific and societal breakthrough for women.
As you can see, the debate is complicated. While many organizations are pushing the pill in order to give women the first libido pill, others are hesitant that there is not enough data for women to make informed decisions about taking the pill. The FDA is set to make its final decision on or before August 18th.
Sources:
FDA
NPR
New York Times
Sprout Pharmaceuticals
Forbes
Science Alert
 Young and middle-age women whose diet included high levels of anthocyanins -- the flavonoids present in red and blue fruits such as strawberries and blueberries -- had a significantly reduced risk for myocardial infarction (MI), a large prospective study found. Women whose anthocyanin intake was in the highest quintile had a 32% decrease in risk of MI during 18 years of follow-up, according to Eric B. Rimm, ScD, of Harvard University, and colleagues. And in a food-based analysis, women who consumed more than three servings of strawberries or blueberries each week showed a trend towards a lower MI risk, with a 34% decrease compared with women who rarely included these fruits in their diet, the researchers reported online in Circulation.
Young and middle-age women whose diet included high levels of anthocyanins -- the flavonoids present in red and blue fruits such as strawberries and blueberries -- had a significantly reduced risk for myocardial infarction (MI), a large prospective study found. Women whose anthocyanin intake was in the highest quintile had a 32% decrease in risk of MI during 18 years of follow-up, according to Eric B. Rimm, ScD, of Harvard University, and colleagues. And in a food-based analysis, women who consumed more than three servings of strawberries or blueberries each week showed a trend towards a lower MI risk, with a 34% decrease compared with women who rarely included these fruits in their diet, the researchers reported online in Circulation.
 The truth is, finding accurate information about reproductive health is hard! Indeed, as Ruth Miller, retired sexual health educator, describes it, "women don't understand their fertility," and know that they have periods but don't know about what happens between their periods. For instance, women have a clear, watery discharge before their period--this is called cervical mucus, but few reproductive health books and professionals tend to talk to women about it.
The truth is, finding accurate information about reproductive health is hard! Indeed, as Ruth Miller, retired sexual health educator, describes it, "women don't understand their fertility," and know that they have periods but don't know about what happens between their periods. For instance, women have a clear, watery discharge before their period--this is called cervical mucus, but few reproductive health books and professionals tend to talk to women about it. Eating disorders, such as anorexia and bulimia, still continue to be a serious problem, especially in women. According to the National Alliance for the Mentally Ill (2003) 90 percent of individuals with eating disorders are women between the ages of 12 and 25. Eating disorders are closely correlated with depression, substance abuse, and anxiety disorders, so it is important to diagnose and treat early.
Eating disorders, such as anorexia and bulimia, still continue to be a serious problem, especially in women. According to the National Alliance for the Mentally Ill (2003) 90 percent of individuals with eating disorders are women between the ages of 12 and 25. Eating disorders are closely correlated with depression, substance abuse, and anxiety disorders, so it is important to diagnose and treat early.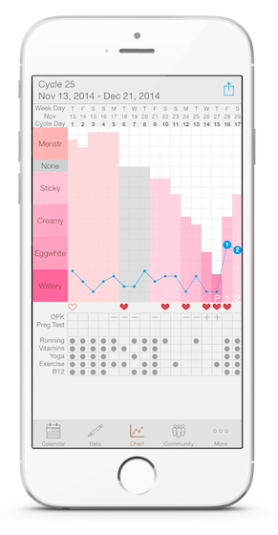
 When patients undergo an acute myocardial infarction, lifestyle changes are necessary to reduce the risk of relapse. Yet research shows that women and minority patients have a more difficult time with risk factor modification efforts. A 2013 study published in the
When patients undergo an acute myocardial infarction, lifestyle changes are necessary to reduce the risk of relapse. Yet research shows that women and minority patients have a more difficult time with risk factor modification efforts. A 2013 study published in the  Everyone wrinkles at the same rate and there’s not really much we can do to prevent it, right? Wrong. There are certain habits that can help you avoid premature wrinkles, making your skin look younger (and healthier) longer. Tanning is one of the leading causes of premature wrinkles. When you go tanning, ultraviolet rays are penetrating deep layers of the skin, weakening the skin’s support structure. Wearing lotion with SPF 15 or higher will help protect your skin, and should become part of your routine. Smoking also accelerates the skin’s aging process, and early wrinkling has been found in smokers as young as 20! The smoke from tobacco also turns the skin an unhealthy color and texture, so the best thing you can do for your skin and your body is to quit smoking!
Everyone wrinkles at the same rate and there’s not really much we can do to prevent it, right? Wrong. There are certain habits that can help you avoid premature wrinkles, making your skin look younger (and healthier) longer. Tanning is one of the leading causes of premature wrinkles. When you go tanning, ultraviolet rays are penetrating deep layers of the skin, weakening the skin’s support structure. Wearing lotion with SPF 15 or higher will help protect your skin, and should become part of your routine. Smoking also accelerates the skin’s aging process, and early wrinkling has been found in smokers as young as 20! The smoke from tobacco also turns the skin an unhealthy color and texture, so the best thing you can do for your skin and your body is to quit smoking!
 You may have heard the buzz this summer about the little pink flibanserin pill, an experimental drug that has been created to boost female libido. This pill, made by Sprout Pharmaceuticals, is the first drug that has claimed to boost female sexual desire and has sparked intense and emotional debates about whether or not the U.S. Food and Drug Administration (FDA) should approve it. The debate has garnered a lot of media attention and public response, all of which can be confusing and misleading depending on the source. We’re here to synthesize the information.
You may have heard the buzz this summer about the little pink flibanserin pill, an experimental drug that has been created to boost female libido. This pill, made by Sprout Pharmaceuticals, is the first drug that has claimed to boost female sexual desire and has sparked intense and emotional debates about whether or not the U.S. Food and Drug Administration (FDA) should approve it. The debate has garnered a lot of media attention and public response, all of which can be confusing and misleading depending on the source. We’re here to synthesize the information. By Rachel Lombard
By Rachel Lombard “Remember to wipe front to back.” “Always pee after having sex.” “Drink lots of cranberry juice!” You’ve probably heard all of these tips before. But what are people trying to help you prevent? The answer is simple: urinary tract infections (UTIs).
“Remember to wipe front to back.” “Always pee after having sex.” “Drink lots of cranberry juice!” You’ve probably heard all of these tips before. But what are people trying to help you prevent? The answer is simple: urinary tract infections (UTIs).