 There is a lot of information on the web promoting various diets for interstitial cystitis (IC), a painful bladder condition with many different symptoms. Both the IC clinical guidelines of the American Urological Association (AUA) and the chronic pelvic pain practice bulletin of the American College of Obstetrical Gynecology (ACOG) recommend dietary modification as a useful approach for helping to manage IC and chronic pelvic pain.
There is a lot of information on the web promoting various diets for interstitial cystitis (IC), a painful bladder condition with many different symptoms. Both the IC clinical guidelines of the American Urological Association (AUA) and the chronic pelvic pain practice bulletin of the American College of Obstetrical Gynecology (ACOG) recommend dietary modification as a useful approach for helping to manage IC and chronic pelvic pain.
However, research into the link between IC and food is very limited. At this time, there is no special “IC Diet.”
IC affects 3-8 million women in the U.S. Men also have it but to a smaller degree, an estimated 1-4 million. However, in men, it is often mistaken for chronic prostatitis. Research has found that there is a lot of variability among IC patients. Some people with IC report that certain foods appear to irritate their bladders and cause painful IC flares. And they find that making a few strategic changes to what they eat and drink can help to control IC symptoms including pain, frequency, and urgency. Other IC patients find that diet does affect their flares.
Some 2,100 IC patients responded to a survey conducted by the Interstitial Cystitis Association (ICA) on complementary and alternative medicines (CAM). Diet topped the list of helpful CAM treatments. The ICA distinguished between looking for and eliminating your individual food triggers and strictly eliminating all the foods on a given “IC Diet” food list. Results were the same in both cases, strongly suggesting that you can eat happy and healthy with a wide variety of items in your diet and still keep your symptoms at bay. The survey also found that newly diagnosed patients find diet changes significantly more helpful than long-standing IC patients.
The ICA recommends eating a healthy, balanced diet. Meet with a registered dietitian (RD) to learn more about how to identify which foods and beverages might bother your IC. Also, find out if your health insurance covers the cost of nutrition counseling.
What We Know about IC & Diet
What to Eat—and What Not to Eat
Differing Approaches on IC & Diet
Source: Interstitial Cystitis Association

 Overweight women with low Vitamin D levels who lose more than 15% of their body weight experience a significant increase in levels of this nutrient, according to a new study by researchers at Fred Hutchinson Cancer Center. "Since vitamin D is generally lower in persons with obesity, it is possible that low vitamin D could account, in part, for the link between obesity and diseases such as cancer, heart disease and diabetes," said Caitlin Mason, PhD, lead author of the study published in the
Overweight women with low Vitamin D levels who lose more than 15% of their body weight experience a significant increase in levels of this nutrient, according to a new study by researchers at Fred Hutchinson Cancer Center. "Since vitamin D is generally lower in persons with obesity, it is possible that low vitamin D could account, in part, for the link between obesity and diseases such as cancer, heart disease and diabetes," said Caitlin Mason, PhD, lead author of the study published in the  When people finish treatment for cancer, they want to bounce back to their former vital selves as quickly as possible. But a new Northwestern Medicine study -- one of the largest survivor studies ever conducted – shows many survivors still suffer moderate to severe problems with pain, fatigue, sleep, memory and concentration three to five years after treatment has ended.
When people finish treatment for cancer, they want to bounce back to their former vital selves as quickly as possible. But a new Northwestern Medicine study -- one of the largest survivor studies ever conducted – shows many survivors still suffer moderate to severe problems with pain, fatigue, sleep, memory and concentration three to five years after treatment has ended. A recent
A recent  Vermont Gov. Peter Shumlin recently signed into law legislation requiring health care insurance policies to cover midwifery services and home births. Supporters of the law said this law is critical in improving access to comprehensive health services for women, reducing system costs and strengthening the quality of care that mothers receive during pregnancy and childbirth.
Vermont Gov. Peter Shumlin recently signed into law legislation requiring health care insurance policies to cover midwifery services and home births. Supporters of the law said this law is critical in improving access to comprehensive health services for women, reducing system costs and strengthening the quality of care that mothers receive during pregnancy and childbirth.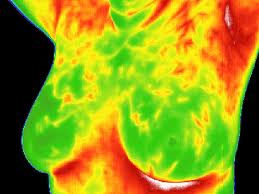 Today, June 2, 2011, the U.S. Food and Drug Administration (FDA) warned women not to substitute breast thermography for mammography to screen for breast cancer. Some health care providers are promoting breast thermography on their websites and claiming that thermography is superior to mammography as a screening method for breast cancer, because it does not require radiation exposure or breast compression.
Today, June 2, 2011, the U.S. Food and Drug Administration (FDA) warned women not to substitute breast thermography for mammography to screen for breast cancer. Some health care providers are promoting breast thermography on their websites and claiming that thermography is superior to mammography as a screening method for breast cancer, because it does not require radiation exposure or breast compression. In 2009, a total of 409,840 infants were born to 15−19 year olds, for a live birth rate of 39.1 per 1,000 women in this age group. Nearly two-thirds of births to women younger than age 18 and more than half of those among 18−19 year olds are unintended. The US teen birth rate fell by more than one-third from 1991 through 2005, but then increased by 5 percent over two consecutive years. Data for 2008 and 2009, however, indicate that the long-term downward trend has resumed. The U.S. teen pregnancy and birth, sexually transmitted diseases (STDs), and abortion rates are substantially higher than those of other western industrialized nations.
In 2009, a total of 409,840 infants were born to 15−19 year olds, for a live birth rate of 39.1 per 1,000 women in this age group. Nearly two-thirds of births to women younger than age 18 and more than half of those among 18−19 year olds are unintended. The US teen birth rate fell by more than one-third from 1991 through 2005, but then increased by 5 percent over two consecutive years. Data for 2008 and 2009, however, indicate that the long-term downward trend has resumed. The U.S. teen pregnancy and birth, sexually transmitted diseases (STDs), and abortion rates are substantially higher than those of other western industrialized nations. Fruits and vegetables are an important part of a healthy diet. Your local markets carry an amazing variety of fresh fruits and vegetables that are both nutritious and delicious. Previous blogs on this site have discussed ways to reduce your risks due to agricultural toxins in pesticides. As you enjoy fresh produce, it is also important to handle these products safely in order to reduce the risks of foodborne illness.
Fruits and vegetables are an important part of a healthy diet. Your local markets carry an amazing variety of fresh fruits and vegetables that are both nutritious and delicious. Previous blogs on this site have discussed ways to reduce your risks due to agricultural toxins in pesticides. As you enjoy fresh produce, it is also important to handle these products safely in order to reduce the risks of foodborne illness.
 A long awaited assessment of potential biomarkers for detecting early ovarian cancer shows that elevated levels of the CA-125 protein still remains the best predictor of disease progression. The CA-125 test has been around for several decades and can help determine the effectiveness of cancer treatments in patient with ovarian cancer, but it is not very useful as a screening tool. A report released in March in Cancer Prevention Research indicated none of the 28 potential serum markers tested in the study outperformed the CA-125.
A long awaited assessment of potential biomarkers for detecting early ovarian cancer shows that elevated levels of the CA-125 protein still remains the best predictor of disease progression. The CA-125 test has been around for several decades and can help determine the effectiveness of cancer treatments in patient with ovarian cancer, but it is not very useful as a screening tool. A report released in March in Cancer Prevention Research indicated none of the 28 potential serum markers tested in the study outperformed the CA-125.