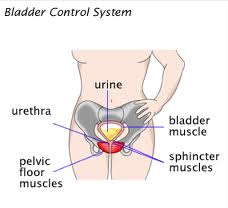
 Loss of bladder control, or urinary incontinence, is a problem that millions of women face. The involuntary loss of urine can range in presentation; it can be minimal, from a few drops when you laugh, exercise, or cough. Or, it can be an accident when you suddenly urge to urinate and can't keep it in. Most episodes of urinary incontinence are the result of altered pressures or stress on the muscles and nerves that help you pass or hold urine in. Hormone changes can also affect muscle strength. Like your vaginal tissue, the muscle tissue in and surrounding the bladder and urethra (the short tube that passes urine from the bladder out the body) requires estrogen to remain supple and strong. When estrogen levels drop in menopause, the tissue around the bladder and urethra thin and weaken,which can lead to incontinence.
Loss of bladder control, or urinary incontinence, is a problem that millions of women face. The involuntary loss of urine can range in presentation; it can be minimal, from a few drops when you laugh, exercise, or cough. Or, it can be an accident when you suddenly urge to urinate and can't keep it in. Most episodes of urinary incontinence are the result of altered pressures or stress on the muscles and nerves that help you pass or hold urine in. Hormone changes can also affect muscle strength. Like your vaginal tissue, the muscle tissue in and surrounding the bladder and urethra (the short tube that passes urine from the bladder out the body) requires estrogen to remain supple and strong. When estrogen levels drop in menopause, the tissue around the bladder and urethra thin and weaken,which can lead to incontinence.
The most common types of urinary incontinence include stress incontinence and urge incontinence. Stress incontinence occurs when the pressures from activities such as laughing, coughing, and sneezing cause leakage. Urge incontinence occurs when you have the urge to urinate and your bladder squeezes at the wrong time. Often, these two types can create a mixed picture. Other bladder problems that can happen are nocturia, when you must wake up multiple times throughout the night to urinate, and dysuria, painful urination.
If you think you have incontinence, visit a professional to learn more about the variety of options you have for treatment. A professional can be your primary care physician, gynecologist, urologist, and even a urogynecologist. Your physician may recommend lifestyle changes such as limiting alcohol or caffeine intake, recording a voiding diary, or strengthening your pelvic floor muscles with Kegel exercises. Beyond this, therapies also include devices inserted into the vagina to hold up the bladder (pessaries), a variety of medications, and surgery if necessary. Your physician will also be the one to exclude other potential causes of bladder problems including infection and neurological damage.
To learn more about urinary issues or other symptomatology that arise during menopause, visit Northwestern's menopause website here.

 A type of exercise called pelvic floor muscle training is effective for treating adult women with urinary incontinence (the involuntary loss of urine) without risk of side effects, according to a new report from the U.S. Agency for Healthcare Research and Quality (AHRQ). The report also found that drug-based treatments can be effective, but the degree of benefit is low and side effects are common.
A type of exercise called pelvic floor muscle training is effective for treating adult women with urinary incontinence (the involuntary loss of urine) without risk of side effects, according to a new report from the U.S. Agency for Healthcare Research and Quality (AHRQ). The report also found that drug-based treatments can be effective, but the degree of benefit is low and side effects are common. The FDA approved Botox injection to treat urinary incontinence (UI) in people with neurologic bladder conditions such as spinal cord injury and multiple sclerosis who have over activity of the bladder. The effectiveness of Botox to treat this type of incontinence was demonstrated in two clinical studies involving 691 patients. Both studies showed statistically significant decreases in the weekly frequency of incontinence episodes in the Botox group compared with placebo.
The FDA approved Botox injection to treat urinary incontinence (UI) in people with neurologic bladder conditions such as spinal cord injury and multiple sclerosis who have over activity of the bladder. The effectiveness of Botox to treat this type of incontinence was demonstrated in two clinical studies involving 691 patients. Both studies showed statistically significant decreases in the weekly frequency of incontinence episodes in the Botox group compared with placebo.