 A study by researchers at the National Institutes of Health (NIH) and the University of Oxford supports the widespread belief that stress may reduce a woman's chance of becoming pregnant. The study is the first of its kind to document, among women without a history of fertility problems, an association between high levels of a substance that is indicative of stress and a reduced chance of becoming pregnant.
A study by researchers at the National Institutes of Health (NIH) and the University of Oxford supports the widespread belief that stress may reduce a woman's chance of becoming pregnant. The study is the first of its kind to document, among women without a history of fertility problems, an association between high levels of a substance that is indicative of stress and a reduced chance of becoming pregnant.
The researchers showed that women who had higher levels of alpha-amylase were less likely to get pregnant than were women with lower levels of the substance. Alpha-amylase is secreted into saliva by the parotid gland, the largest of the salivary glands. Although alpha-amylase digests starch, in recent years it has been used as a barometer of the body's response to physical or psychological stress. The substance is secreted when the nervous system produces catecholamines, compounds that initiate a type of stress response.
Researchers tracked the ovulation cycles of 274 English women ages 18-40 who were trying to conceive. On the sixth day of their cycles, each woman collected a sample of her saliva, which was subsequently tested for alpha-amylase. The researchers found that, all other factors being equal, women with high alpha-amylase levels were less likely to conceive than were women with low levels. A larger study is currently underway to confirm these findings. If these finding hold up, health providers will need to find appropriate ways to help women alleviate stress while trying to conceive.
To view the NIH Press release, click here.

 Study finds association between stress level in early cycle, severity of symptoms
Study finds association between stress level in early cycle, severity of symptoms The most recent statistics on the women who participate in our
The most recent statistics on the women who participate in our 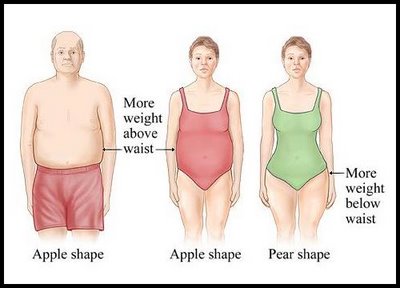 CHICAGO --- The more an older woman weighs, the worse her memory, according to new research from Northwestern Medicine. The effect is more pronounced in women who carry excess weight around their hips, known as pear shapes, than women who carry it around their waists, called apple shapes. The study of 8,745 cognitively normal, post-menopausal women ages 65 to 79 from the Women's Health Initiative hormone trials is the first in the United States to link obesity to poorer memory and brain function in women and to identify the body-shape connection.
CHICAGO --- The more an older woman weighs, the worse her memory, according to new research from Northwestern Medicine. The effect is more pronounced in women who carry excess weight around their hips, known as pear shapes, than women who carry it around their waists, called apple shapes. The study of 8,745 cognitively normal, post-menopausal women ages 65 to 79 from the Women's Health Initiative hormone trials is the first in the United States to link obesity to poorer memory and brain function in women and to identify the body-shape connection.
 According to the World Health Organization, alcohol is one of the most significant risk factors for diseases including chronic conditions like cancer, diabetes, and heart disease. Compared with men, women become more cognitively impaired by alcohol and are more susceptible to alcohol-related organ damage. Women develop damage with less intake and over a shorter period of time than men. When men and women of the same weight consume equal amounts of alcohol, women have higher blood alcohol concentrations. This is due in part because women have proportionately more body fat and a lower volume of body water compared with men of similar weight. This leads to women having a higher concentration of alcohol because there is less volume of water to dilute the alcohol.
According to the World Health Organization, alcohol is one of the most significant risk factors for diseases including chronic conditions like cancer, diabetes, and heart disease. Compared with men, women become more cognitively impaired by alcohol and are more susceptible to alcohol-related organ damage. Women develop damage with less intake and over a shorter period of time than men. When men and women of the same weight consume equal amounts of alcohol, women have higher blood alcohol concentrations. This is due in part because women have proportionately more body fat and a lower volume of body water compared with men of similar weight. This leads to women having a higher concentration of alcohol because there is less volume of water to dilute the alcohol. You may have seen the cover article on our Spring Newsletter titled “Spotlight on Obesity: Is it just your weight?” This article focuses not only on the epidemic of obesity in the U.S. but also on the serious health conditions that may result from obesity. Although obesity is on the rise, however, eating disorders such as anorexia and bulimia still continue to be a problem, especially in women. According to the National Alliance for the Mentally Ill (2003) 90 percent of individuals with eating disorders are women between the ages of 12 and 25. Eating disorders are closely correlated with depression, substance abuse, and anxiety disorders, so it is important to diagnose and treat early.
You may have seen the cover article on our Spring Newsletter titled “Spotlight on Obesity: Is it just your weight?” This article focuses not only on the epidemic of obesity in the U.S. but also on the serious health conditions that may result from obesity. Although obesity is on the rise, however, eating disorders such as anorexia and bulimia still continue to be a problem, especially in women. According to the National Alliance for the Mentally Ill (2003) 90 percent of individuals with eating disorders are women between the ages of 12 and 25. Eating disorders are closely correlated with depression, substance abuse, and anxiety disorders, so it is important to diagnose and treat early. In recognition of Poison Prevention Week (March 14-20), the Center for Disease Control (CDC) is highlighting the growing issue of unintentional drug poisoning in the United States. More than 26,000 deaths from unintentional drug poisoning occurred in the U.S. in 2006. Opioid pain medications (e.g., oxycodones and methadone) were involved in more than half of these deaths. In recent years, this cause of death has more than doubled between 1999 and 2006. In 2006, 17,740 drug overdose deaths occurred among males and 8,660 among females. Male rates exceed females rates in every age group. However, male rates have doubled and female rates have nearly tripled since 1999. In response to this growing problem the CDC has developed an issue brief titled
In recognition of Poison Prevention Week (March 14-20), the Center for Disease Control (CDC) is highlighting the growing issue of unintentional drug poisoning in the United States. More than 26,000 deaths from unintentional drug poisoning occurred in the U.S. in 2006. Opioid pain medications (e.g., oxycodones and methadone) were involved in more than half of these deaths. In recent years, this cause of death has more than doubled between 1999 and 2006. In 2006, 17,740 drug overdose deaths occurred among males and 8,660 among females. Male rates exceed females rates in every age group. However, male rates have doubled and female rates have nearly tripled since 1999. In response to this growing problem the CDC has developed an issue brief titled 

