The need for health care varies greatly over a lifespan, with older adults having significantly more health-related needs and costs than younger individuals. Women, in particular, often face a myriad of health problems as they transition through menopause. Sadly, despite the fact that every woman will go through menopause, very little is understood about the physical and mental changes that occur during this period of life. In addition, women may struggle to find pharmaceutical solutions, which can safely provide proven relief without the worry that those available will increase their likelihood of other health and mental complications.
Much is misunderstood about menopause and the changes that are associated with the hormonal fluctuations. This is largely due to the fact this inevitable transition is rarely apart of the conversation, particularly in the context of health care. Further, menopause is expected to be merely “bothersome”; not something one could attribute real health problems to. Although maternity care and issues related to younger women are required in the Affordable Care Act as essential health benefits, nothing of legislative note will improve the knowledge and acceptance of this natural life progression.
Most insurance companies do not even cover basic medications associated with menopausal symptoms, and conflicting research has women scared about the potential long-term effects associated with hormone replacement therapy. Negative press, little medical literature and low financial assistance often leaves women to suffer through menopause silently, many of whom worry constantly about memory deficits they experience and potential long term changes.
A recent study focused on the memory complaints of midlife women has been receiving a lot of attention. The study, conducted at the University of Illinois- at Chicago (UIC), attempted to determine if women who are experiencing hot flushes during menopause were able to accurately predict their own memory performance.
According to the principal author, Lauren Drogos, “We found that a one-item question: ‘How would you rate your memory in terms of the kinds of problems that you have?’ was the best predictor of verbal memory performance on a list-learning task. We also found that many complaints were related to mood symptoms.”
In the US, the average woman becomes postmenopausal around the age of 51. Common symptoms that occur include hot flushes, sleep disturbances, mood changes and memory problems. However, until recently it was believed that women were unable to accurately describe the current state of their memory and the changes they experience as they progress through menopause.
Despite the difficulty in being taken seriously about the physical and mental challenges that menopause presents, this recent study from Drogos, along with other research, shows that woman are able to accurately describe their current memory abilities. Specifically, a group of sixty-eight women performed a series of memory tests and were then asked, to detail the types of memory problems they were experiencing. The study concluded that women were able to accurately rank themselves on a scale from no memory problems to severe problems.
Using recall of a short story, the deficits seen in memory did not indicate that women were suffering from dementia, nor were they experiencing shortfalls in memory that were impacting daily life. Instead, it was simply indicative that women who experienced memory deficits often recognized the changes occurring.
Previous research focusing on women’s transitions through menopause also found that hot flushes during the nighttime were the best predictors of memory performance in women. This leads researchers within the Women’s Mental Health Research Program at UIC, to believe that sleep disturbances and stress hormones may play integral roles in memory and hot flushes.
The good news for women concerned about the transition through menopause is that the cognitive decline that occurs appears to only be temporary, with performance rebounding early into post-menopause. Further, for those who want to keep both their minds and bodies at peak performance, research indicates that leading a non-sedentary lifestyle, keeping mentally active, and having a healthy diet can be the best preventers of cognitive decline. To learn more about menopause, visit menopausenu.org, a new web site that helps women evaluate their overall health and menopause symptoms.

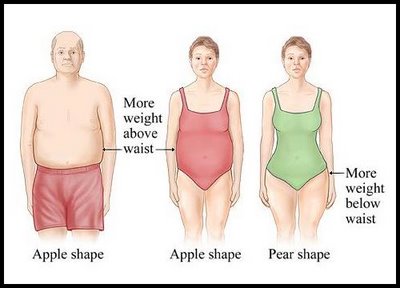 CHICAGO --- The more an older woman weighs, the worse her memory, according to new research from Northwestern Medicine. The effect is more pronounced in women who carry excess weight around their hips, known as pear shapes, than women who carry it around their waists, called apple shapes. The study of 8,745 cognitively normal, post-menopausal women ages 65 to 79 from the Women's Health Initiative hormone trials is the first in the United States to link obesity to poorer memory and brain function in women and to identify the body-shape connection.
CHICAGO --- The more an older woman weighs, the worse her memory, according to new research from Northwestern Medicine. The effect is more pronounced in women who carry excess weight around their hips, known as pear shapes, than women who carry it around their waists, called apple shapes. The study of 8,745 cognitively normal, post-menopausal women ages 65 to 79 from the Women's Health Initiative hormone trials is the first in the United States to link obesity to poorer memory and brain function in women and to identify the body-shape connection.