 Researchers have identified a key step in the establishment of a pregnancy. The discovery may shed light on fertility disorders and diseases of the uterus, including endometrial cancer. At the start of each menstrual cycle, levels of the hormone estrogen begin to rise, which causes the uterine lining to grow and thicken. When the ovary releases an egg, levels of another hormone, progesterone, increase. Higher progesterone levels put the brakes on the estrogen-driven growth of the uterine lining, allowing the lining to mature and egg implantation to take place. Because of this function, progesterone is sometimes given to women to treat infertility and prevent premature birth. However, it carries some unpleasant side effects. A greater understanding of how progesterone works could lead to better treatments. It could also shed light on disorders such as endometrial cancer and endometriosis, which is marked by uncontrolled growth of the uterine lining. To clarify how progesterone stops the growth of the uterine lining, the study's first author, Dr. Quanxi Li of the University of Illinois at Urbana-Champaign, led a group of researchers from several institutions. Their findings were published in the February 28, 2011, issue of Science. The team focused on the role of a protein called Hand2 in halting the growth of the uterine lining. They had previously found that blocking the progesterone receptor decreased Hand2 expression in uterine cells, indicating a link between Hand2 and progesterone.In their new study, the team genetically engineered mice to lack Hand2 in the uterus, and then gave them progesterone. They then stimulated uterine lining growth with estrogen. In normal mice, progesterone prevents the uterine lining from growing. In the mice without Hand2, however, the lining grew in spite of the progesterone treatment. The scientists found that uterine cells beneath the lining express Hand2 during egg implantation. Further experiments revealed that estrogen stimulates the production of molecules called growth factors, which cause the uterine lining to grow. High levels of Hand2, brought on by progesterone, stop the production of these growth factors. Therefore, the uterine lining stops growing, allowing egg implantation. The discovery of Hand2's role in halting growth of the uterine lining may spur development of treatments for diseases like endometriosis and endometrial cancer. "This information helps us understand how the interplay of hormones prepares the uterus to host and support the embryo as it grows," says Dr. Milan Bagchi, a senior author of the study. "Our next priority will be to examine whether Hand2 plays a critical role in the human uterus as well." Related Links: Pregnancy Infertility Endometriosis Source: National Institutes of Health
Researchers have identified a key step in the establishment of a pregnancy. The discovery may shed light on fertility disorders and diseases of the uterus, including endometrial cancer. At the start of each menstrual cycle, levels of the hormone estrogen begin to rise, which causes the uterine lining to grow and thicken. When the ovary releases an egg, levels of another hormone, progesterone, increase. Higher progesterone levels put the brakes on the estrogen-driven growth of the uterine lining, allowing the lining to mature and egg implantation to take place. Because of this function, progesterone is sometimes given to women to treat infertility and prevent premature birth. However, it carries some unpleasant side effects. A greater understanding of how progesterone works could lead to better treatments. It could also shed light on disorders such as endometrial cancer and endometriosis, which is marked by uncontrolled growth of the uterine lining. To clarify how progesterone stops the growth of the uterine lining, the study's first author, Dr. Quanxi Li of the University of Illinois at Urbana-Champaign, led a group of researchers from several institutions. Their findings were published in the February 28, 2011, issue of Science. The team focused on the role of a protein called Hand2 in halting the growth of the uterine lining. They had previously found that blocking the progesterone receptor decreased Hand2 expression in uterine cells, indicating a link between Hand2 and progesterone.In their new study, the team genetically engineered mice to lack Hand2 in the uterus, and then gave them progesterone. They then stimulated uterine lining growth with estrogen. In normal mice, progesterone prevents the uterine lining from growing. In the mice without Hand2, however, the lining grew in spite of the progesterone treatment. The scientists found that uterine cells beneath the lining express Hand2 during egg implantation. Further experiments revealed that estrogen stimulates the production of molecules called growth factors, which cause the uterine lining to grow. High levels of Hand2, brought on by progesterone, stop the production of these growth factors. Therefore, the uterine lining stops growing, allowing egg implantation. The discovery of Hand2's role in halting growth of the uterine lining may spur development of treatments for diseases like endometriosis and endometrial cancer. "This information helps us understand how the interplay of hormones prepares the uterus to host and support the embryo as it grows," says Dr. Milan Bagchi, a senior author of the study. "Our next priority will be to examine whether Hand2 plays a critical role in the human uterus as well." Related Links: Pregnancy Infertility Endometriosis Source: National Institutes of Health
 A higher proportion of women on a company’s board leads to greater opportunities at the executive level for women, according to new research. Despite continued gains in low- to mid-level management positions, women still struggle to break through the corporate glass ceiling and attain coveted top-management positions. Today, women account for nearly half of the nation’s overall workforce, but hold only 6 percent of corporate CEO and high-level executive roles. New research from the Kellogg School at Northwestern finds that one key to women’s career advancement may lie in the gender makeup of a company’s corporate board.
A higher proportion of women on a company’s board leads to greater opportunities at the executive level for women, according to new research. Despite continued gains in low- to mid-level management positions, women still struggle to break through the corporate glass ceiling and attain coveted top-management positions. Today, women account for nearly half of the nation’s overall workforce, but hold only 6 percent of corporate CEO and high-level executive roles. New research from the Kellogg School at Northwestern finds that one key to women’s career advancement may lie in the gender makeup of a company’s corporate board.
The research examines female representation on corporate boards and its subsequent effect on the gender composition of the company’s top management positions. According to the study, a higher representation of women on a company’s board of directors directly increases the female share of and access to higher positions within the company.
“Unfortunately, there are still institutional gender barriers in today’s workplace that prevent women from holding high-level executive positions,” said David Matsa, assistant professor of finance. “Our research uncovers the impact of ‘women helping women’ at the highest level of company leadership. Women who hold board positions have a unique opportunity to propel their female colleagues into executive roles, so in effect, when women’s share of board seats increases, their share of top-level positions also increases.”
Matsa, with co-author Amalia Miller of the University of Virginia and the RAND Corporation, a nonprofit research organization, analyzed data about corporate board members and top executives for a large panel of publicly traded companies from 1997 to 2009.
“In addition, we found that as a board’s gender composition evolved and increased its number of female seats, over time the likelihood that these boards would select female managers also increased,” said Matsa. “However, this gender shift can take multiple years. Our research shows that while the female share of board seats may increase the desire to hire other female executives, there is a lag time for women to achieve these roles, probably because the positions are currently occupied by qualified candidates.”
Interestingly, the researchers noted that the reverse situation is not true: Having female executives in top roles did not impact the gender makeup of corporate boards over time. This implies that female board membership typically precedes shifts in executive positions held by women, but not vice versa.
“Overall, the results show that women are each other’s best advocates, and by helping one another they have the potential to make remarkable gains in today’s workforce,” said Matsa. “When women are seated at the highest levels in corporate America, they are in a unique position to serve as mentors to those below them and to create more opportunities for female leadership and management roles.”
The study, “Chipping Away at the Glass Ceiling: Gender Spillovers in Corporate Leadership,” will be published in the May 2011 issue of The American Economic Review: Papers and Proceedings.
 Women, on average, live one-third of their lives post menopause. Some women find menopause an easy transition. Other women are chronically bothered by persistent hot flashes and night sweats that impact their quality of life. For years, hormone therapy was the answer but it has been shadowed by controversy as researchers learn more about estrogen and its long term impact on the body. The Institute for Women's Health Research discussed this controversy in its March e-newsletter that is available at ENewsletter March 2011final.
Women, on average, live one-third of their lives post menopause. Some women find menopause an easy transition. Other women are chronically bothered by persistent hot flashes and night sweats that impact their quality of life. For years, hormone therapy was the answer but it has been shadowed by controversy as researchers learn more about estrogen and its long term impact on the body. The Institute for Women's Health Research discussed this controversy in its March e-newsletter that is available at ENewsletter March 2011final.
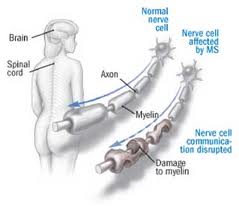 Multiple sclerosis (MS) disrupts communication between the brain and other parts of the body. In the worst cases, it can bring partial or complete paralysis. Researchers don’t yet know what causes this disease or how to cure it, but they’ve been making progress on both fronts.
Multiple sclerosis (MS) disrupts communication between the brain and other parts of the body. In the worst cases, it can bring partial or complete paralysis. Researchers don’t yet know what causes this disease or how to cure it, but they’ve been making progress on both fronts.
Symptoms of MS arise most often between the ages of 20 and 40. It often begins with blurred or double vision, color distortion, or even blindness in one eye. It can cause muscle weakness, vision loss, numbness or tingling, and difficulty with coordination and balance. MS can bring many other symptoms as well.
In some people, doctors may not be able to readily identify the cause of these symptoms. Patients may endure years of uncertainty and multiple diagnoses while baffling symptoms come and go. The vast majority of patients are mildly affected, but in the worst cases, MS can leave a person unable to write, speak or walk.
MS is a disease in which the body’s immune system inappropriately attacks the brain and spinal cord. Specifically, the immune system targets the fatty insulating material around nerves called myelin. When myelin is damaged, the messages that nerve cells send and receive can be interrupted.
Researchers estimate that 250,000 to 350,000 people in the United States have been diagnosed with MS. Scientists don’t yet understand what triggers the immune system to attack myelin in these people. But researchers do know that whites are more than twice as likely as others to develop MS, and women almost twice as likely as men.
Geography seems to play a role in MS. The disease is much more prevalent in temperate climates than in tropical regions. Your risk for MS seems to depend on where you live before the age of 15. Some studies have found that a person who moves before the age of 15 tends to adopt the risk of the new area. People moving after age 15 seem to maintain the risk level of the area where they grew up. Some researchers believe that vitamin D, which the body makes when sunlight strikes the skin, may lower the risk of MS and help explain these findings, but studies haven’t yet confirmed this link.
Some microbes, such as the Epstein-Barr virus, have been suspected of causing MS. But researchers haven’t been able to prove for certain that any microbes raise your chances of getting MS. Cigarette smoking, however, does appear to raise your risk.
Genes clearly affect how likely you are to develop MS. Having a sibling with MS raises your risk of getting MS to about 4% to 5%; having an identical twin raises your risk to about 25% to 30%. These facts suggest a strong genetic component to MS. However, although some studies have linked specific genes to MS, most of the results haven’t been definitive. Researchers are now working on more detailed studies.
There’s no cure yet for MS, but various therapies can treat it. Researchers are continuing to develop new and better therapies for MS, with several now in the pipeline.
Source: National Institutes of Health
 Pregnant women who are unaware that they have HIV miss the chance for drug treatment that can benefit not only their own health, but could also prevent them from transmitting the virus to their infants. When HIV is not diagnosed until women go into labor, their infants are usually treated soon after birth with the anti HIV drug zidovudine (ZDV), to prevent the infants from becoming infected with the virus.
Pregnant women who are unaware that they have HIV miss the chance for drug treatment that can benefit not only their own health, but could also prevent them from transmitting the virus to their infants. When HIV is not diagnosed until women go into labor, their infants are usually treated soon after birth with the anti HIV drug zidovudine (ZDV), to prevent the infants from becoming infected with the virus.
Now, a National Institutes of Health study has found that adding one or two drugs to the standard ZDV treatment can reduce the chances by more than 50 percent that an infant will develop an HIV infection.
The study results were presented at the Conference on Retroviruses and Opportunistic Infections, in Boston. The study was conducted at research hospitals in Brazil, South Africa, Argentina, and the United States, under contract to the NIH’s Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD).
An estimated one fifth of people in the United States who have HIV are unaware that they harbor the virus. From 100 to 200 infants are born with HIV in the United States each year, many to women who either were not tested in early pregnancy or who did not receive treatment during pregnancy. Internationally, estimates of HIV testing vary, with only 21 percent of pregnant women in low and middle income countries having been tested for HIV during pregnancy.
"To reduce mother-to-child HIV transmission, it's best to begin antiretroviral treatment during pregnancy," said Heather Watts, M.D., a medical officer in NICHD and an author of the study. "However, when treatment during pregnancy isn’t possible, our results show that adding one or two drugs to the current regimen provides another important means to reduce the chance for mother-to-child HIV transmission."
At the 19 participating research sites, the NICHD/ HIV Prevention Trials Network 040 study evaluated 1,684 infants born to women whose HIV infections were not diagnosed until they were in labor. The infants were randomly assigned to three groups: those receiving the standard 6 weeks of therapy with ZDV, those receiving 6 weeks of ZDV plus 3 doses of nevirapine (NVP) during the first week of life, and those receiving 6 weeks of ZDV plus two weeks of lamivudine (3TC) and nelfinavir (NFV). The study results showed that treatment with the two and three drug regimens reduced HIV transmission by more than 50 percent.
"Our results showed conclusively that the two and three drug regimens are superior to the standard treatment with zidovudine," said study chair Karin Nielsen-Saines, M.D., clinical professor of pediatrics at the David Geffen School of Medicine at the University of California at Los Angeles.
To read the entire NIH press release, click HERE.
 Women who have more than two alcoholic drinks a week -- particularly nonlight beer -- appear to be at increased risk of developing the skin condition psoriasis. The cohort study of almost 83,000 nurses -- over 1,000 of whom had cases of incident psoriasis -- found that among women who consumed 2.3 or more alcoholic drinks per week, the relative risk (the ratio of the risk of disease among those exposed to a risk factor to the risk among those not exposed, in this case a RR >1 indicates that there was a higher risk for psoriasis in the drinking group) for psoriasis was 1.72 according to Abrar A. Qureshi, MD, of Harvard University in Boston, and colleagues. Qureshi and co-authors reported their findings in the December Archives of Dermatology.
Women who have more than two alcoholic drinks a week -- particularly nonlight beer -- appear to be at increased risk of developing the skin condition psoriasis. The cohort study of almost 83,000 nurses -- over 1,000 of whom had cases of incident psoriasis -- found that among women who consumed 2.3 or more alcoholic drinks per week, the relative risk (the ratio of the risk of disease among those exposed to a risk factor to the risk among those not exposed, in this case a RR >1 indicates that there was a higher risk for psoriasis in the drinking group) for psoriasis was 1.72 according to Abrar A. Qureshi, MD, of Harvard University in Boston, and colleagues. Qureshi and co-authors reported their findings in the December Archives of Dermatology.
A few retrospective and case-control studies have suggested a possible link between alcohol use and psoriasis, particularly in men, the researchers noted. To see if women's risk of the autoimmune skin disease was associated with alcohol, Qureshi's group analyzed data from the longitudinal Nurses' Health Study II, which began enrolling women in 1989 and periodically questioned them about health and health behaviors.
In 2005, 82,869 participants responded to a questionnaire asking whether they had ever been given a diagnosis of psoriasis; 2,430 women reported that they had.Follow-up for the current analysis began in 1991, the first year for which there was information regarding alcohol intake. During the ensuing years, there were 1,069 incident cases of psoriasis, which were included in the current analysis.
The risk for psoriasis among women who used alcohol remained significant after adjustment for variables including age, body mass index, and physical activity. In addition, the risk for psoriasis increased with greater alcohol intake. The excess risk for psoriasis among women who drank five or more nonlight beers per week was 1.53%.
When the investigators repeated the analysis for those women whose diagnosis of psoriasis was confirmed using the detailed Psoriasis Screening Tool, the risk among those who consumed five or more nonlight beers was 2.3 times higher than nondrinkers. In contrast, there was no significant increase among women who drank other types of alcohol.
The investigators hypothesized that some component in beer -- specifically barley, which contains gluten -- may be responsible for the increased risk, and that more grain is used to manufacture full-strength beer.The link to gluten in beer was supported by the observation that some patients with psoriasis appear to be sensitive to gluten and improve on a gluten-free diet, they noted.
Limitations of the study included reliance on patient recall for a diagnosis of psoriasis, and that the cohort was well-educated and therefore not entirely representative of the entire cohort of women in the Nurses' Health Study.
Source: MedPage Today
 Study finds women who suffer from hot flashes when they begin menopause are at lower risk for cardiovascular events
Study finds women who suffer from hot flashes when they begin menopause are at lower risk for cardiovascular events
You are enjoying a night out with friends when it starts; first you feel flush, then a sensation of warmth crawls down your body. Soon you begin perspiring and you feel as if everyone around you can tell what is happening – another hot flash. An estimated three out of four women experience hot flashes associated with menopause and nearly all would agree they are a nuisance, but experts say there could be an upside to having hot flashes. New research released today in the online edition of the journal Menopause suggests that women who suffer from hot flashes and night sweats may be at lower risk for cardiovascular disease, stroke and death.
“While they are certainly bothersome, hot flashes may not be all bad,” said Emily Szmuilowicz, MD, endocrinologist at Northwestern Medicine and lead author of the study. “Our research found that despite previous reports suggesting that menopause symptoms were associated with increased levels of risk markers for heart disease, such as blood pressure and cholesterol, the actual outcomes tell a different story.”
Szmuilowicz, who co-chaired the study along with JoAnn Manson, MD and Ellen Seely, MD from Harvard Medical School, reviewed medical information from 60,000 women who were enrolled in the Women’s Health Initiative Observational Study and followed for ten years, to determine the relationship between menopause symptoms and cardiovascular events. Subjects were grouped into four categories – women who experienced hot flashes and night sweats at the onset of menopause, later in menopause, during both time periods, and not at all.
“We found that women who experienced symptoms when they began menopause had fewer cardiovascular events than those who experienced hot flashes late in menopause or not at all,” said Szmuilowicz. The results are significant since there has been concern that menopausal symptoms, which result from instability in the blood vessels in the skin, may put women at risk for other types of vascular problems as well.
“It is reassuring that these symptoms, which are experienced by so many women, do not seem to correlate with increased risk of cardiovascular disease,” said Szmuilowicz.
Szmuilowicz and team say more research needs to be done in order to understand the mechanisms behind the association, but say it’s good news for the millions of women who experience these troublesome symptoms at the time of menopause.
“Hot flashes will never be enjoyable, but perhaps these findings will make them more tolerable,” said Szmuilowicz.The paper titled “Vasomotor symptoms and cardiovascular events in postmenopausal women” is now available online and will be printed in the June issue of Menopause. For more information, visit .
Source: Northwestern Memorial Hospital, Chicago
 Maternal cigarette smoking in the first trimester was associated with a 20 to 70 percent greater likelihood that a baby would be born with certain types of congenital heart defects, according to a study by the Centers for Disease Control and Prevention. Congenital heart defects are the most common type of birth defects, contributing to approximately 30 percent of infant deaths from birth defects annually.
Maternal cigarette smoking in the first trimester was associated with a 20 to 70 percent greater likelihood that a baby would be born with certain types of congenital heart defects, according to a study by the Centers for Disease Control and Prevention. Congenital heart defects are the most common type of birth defects, contributing to approximately 30 percent of infant deaths from birth defects annually.
The study found an association between tobacco exposure and certain types of defects such as those that obstruct the flow of blood from the right side of the heart into the lungs (right ventricular outflow tract obstructions) and openings between the upper chambers of the heart (atrial septal defects). The study is in the Feb. 28 issue of the journal Pediatrics.
"Women who smoke and are thinking about becoming pregnant need to quit smoking and, if they're already pregnant, they need to stop," said CDC Director Thomas R. Frieden, M.D., M.P.H. "Quitting is the single most important thing a woman can do to improve her health as well as the health of her baby."
Based on the findings of this and other studies, eliminating smoking before or very early in pregnancy could prevent as many as 100 cases of right ventricular outflow tract obstructions and 700 cases of atrial septal defects each year in the United States. For atrial septal defects alone, that could potentially save $16 million in hospital costs.
"Successfully stopping smoking during pregnancy also lowers the chances of pregnancy complications such as preterm delivery and that an infant will have other complications such as low birth weight," said Adolfo Correa, M.D., Ph.D., medical officer in CDC's National Center on Birth Defects and Developmental Disabilities.
The findings from the study are based on a large population-based case-control study of congenital heart defects conducted in the United States.
Congenital heart defects are conditions present at birth that decrease the ability of the heart to work well, which can result in an increased likelihood of death or long-term disabilities. They affect nearly 40,000 infants in the United States every year.
Click HERE to view the publication.
 Breast-feeding may help reduce some long-term negative side effects of cancer treatment in women who survived childhood cancer, according to a new study.
Breast-feeding may help reduce some long-term negative side effects of cancer treatment in women who survived childhood cancer, according to a new study.
The findings suggest that making women aware of the benefits of breast-feeding should be part of routine recommendations for a post-cancer healthy lifestyle, said Susan W. Ogg and colleagues from St. Jude Children's Research Hospital in Memphis, Tenn.
The researchers reviewed studies that examined whether women can successfully breast-feed after treatment for childhood cancer, how childhood cancer treatment affects women's health in general over the long term and whether breast-feeding might reduce both the risk and impact of treatment-related toxicity in cancer survivors.
The analysis revealed that breast-feeding can have a positive impact on a mother's bone mineral density, metabolic syndrome risk factors, cardiovascular disease and secondary tumors -- health factors that are all negatively affected by childhood cancer.
"Alongside advice to eat plenty of fruit and vegetables, abstain from smoking, use suitable sun protection, practice safe sex and take part in regular physical activity, women who have survived childhood cancer and are physically able to breast-feed should be actively encouraged to do so to help protect them against the many lasting effects of cancer treatment," the researchers concluded.
The study findings were released online in advance of publication in an upcoming print issue of the Journal of Cancer Survivorship.
About 80 percent of U.S. children and teens diagnosed with childhood cancer now survive, but many face major health challenges stemming from the cancer itself or its treatment. These challenges include impaired growth and development, organ dysfunction, reproductive difficulties and risk of cancer recurrence.
SOURCE: Journal of Cancer Survivorship, news release, Jan. 20, 2011
By Robert Preidt
 Painful Hip Fractures Strike Breast Cancer Survivors
Painful Hip Fractures Strike Breast Cancer Survivors
A hip fracture is not common in a 54-year-old woman, unless she is a 54-year-old breast cancer survivor, according to a new Northwestern Medicine study. Researchers found that a combination of early menopause due to breast cancer treatment and common drugs used to treat breast cancer, could be weakening the bones of breast cancer survivors once they hit middle age, leading to hip fractures.
Results of the study are published in the February 2011 issue of Clinical Cancer Research.
Hip fractures are rare in people under 70. Yet, Northwestern Medicine physician Beatrice Edwards, M.D., found that several breast cancer survivors in their early 50s were coming to her for treatment of hip fractures. Edwards is director of the Bone Health and Osteoporosis program and associate professor of medicine and of orthopaedic surgery at Northwestern University Feinberg School of Medicine.
Researchers studied six of these women over one year and assessed the type of breast cancer they had, the treatment they underwent and a hip fracture’s effect on quality of life, said Edwards, lead author of the study.
“One year after the fracture the women still reported difficulty with climbing stairs, shopping and heavy housekeeping,” Edwards said. “Their health care costs may increase and their fractures contribute to losing some independence.”
Edwards was surprised to find that the majority of the women did not have osteoporosis, but did have lower than normal bone mineral density (osteopenia). This suggests that rapid change in bone architecture from chemotherapy, early menopause and adjuvant therapy may not be evident on bone mineral density test, Edwards said.
The women had early-stage breast cancer and received treatment including lumpectomy, radiation therapy and chemotherapy with cytoxan and adriamycin one to four years before the fracture occurred. They were all perimenopausal at the time of the fracture.
Four of the six women had breast cancer that grew in response to estrogen and received aromatase inhibitors (AIs) as part of their cancer therapy to block their bodies from making estrogen. Recent studies have linked AIs with possible bone loss in women. Edwards’ team also reviewed reports from the FDA’s adverse event reporting system and other databases and found that AIs were the most common drug class associated with hip fractures.
“Although the majority of women with breast cancer can expect to be fully cured from the disease, the prevention of cancer treatment-induced bone loss is important to consider in cancer survival,” Edwards said. “More research needs to be done before treatment guidelines are changed, but greater awareness of the adverse effects of certain breast cancer drugs is needed.”
Edwards said the next step is for researchers to conduct a clinical trial and give bone density screenings to women before they enter breast cancer chemotherapy. High-risk patients would be flagged and given preventive bone loss therapy and monitored for premature hip fractures.
“The pain and suffering and hospital stays and higher health costs associated with these hip fractures might be prevented through early intervention,” Edwards said.
The title of the paper is “Cancer therapy associated bone loss: Implications for hip fractures in mid-life women with breast cancer.”
By Erin White, Northwestern Newscenter
