 Sexual violence is a serious public health problem in the United States and world wide! Statistics underestimate the problem because many victims are afraid to tell the police, family, or friends about the violence. In the United States, 1 in 5 women and 1 in 71 men report that they have experienced an attempted or completed rape in their lifetime. In addition, nearly 1 in 2 women and 1 in 5 men report that they have experienced sexual violence victimization other that rape in their lifetime. Globally, one in four women will likely experience sexual violence by an intimate partner and one in three girls report their first sexual experience being forced, according to the World Health Organization (WHO).
Sexual violence is a serious public health problem in the United States and world wide! Statistics underestimate the problem because many victims are afraid to tell the police, family, or friends about the violence. In the United States, 1 in 5 women and 1 in 71 men report that they have experienced an attempted or completed rape in their lifetime. In addition, nearly 1 in 2 women and 1 in 5 men report that they have experienced sexual violence victimization other that rape in their lifetime. Globally, one in four women will likely experience sexual violence by an intimate partner and one in three girls report their first sexual experience being forced, according to the World Health Organization (WHO).
Sexual violence is any sexual activity where consent is not freely given. This includes completed or attempted sex acts that are against the victim's will or involve a victim who is unable to consent. It also includes abusive sexual contact and noncontact sexual abuse (such as verbal sexual harassment). Child sexual abuse is also considered sexual violence.
This type of violence can be committed by anyone - a current or former intimate partner, a family member, a person in position of power or trust, a friend, an acquaintance, someone known only by sight, or a stranger.
Sexual violence impacts health in many ways and can lead to long-term health and emotional problems. Victims may experience chronic pain, headaches, and sexually transmitted diseases. They are often fearful or anxious, and may have problems trusting others. Anger and stress can lead to eating disorders, depression, and even suicidal thoughts.
If you are, or know someone who is, the victim of sexual violence, contact the Rape, Abuse, and Incest National Network (RAINN) hotline at 1-800-656-HOPE or contact your local emergency services at 9-1-1.
Source: Centers for Disease Control and Prevention (CDC)

 Heart disease is the leading cause of death among women, and evidence-based national guidelines promote the use of daily aspirin for women at increased risk for cardiovascular disease. However, less than half of the women who could benefit from aspirin are taking it, according to an article available free online at the
Heart disease is the leading cause of death among women, and evidence-based national guidelines promote the use of daily aspirin for women at increased risk for cardiovascular disease. However, less than half of the women who could benefit from aspirin are taking it, according to an article available free online at the  Have you noticed Salmonella and other food borne illnesses are on the rise---everywhere. While we rely on government agencies to keep our restaurants inspected and food handling industries regulated, at the home level, it's up to us!. The kitchen is the germiest room in the house-- teeming with billions of microorganisms on countertops, refrigerators and cutting boards. And the worse culprit: the kitchen sponge!
Have you noticed Salmonella and other food borne illnesses are on the rise---everywhere. While we rely on government agencies to keep our restaurants inspected and food handling industries regulated, at the home level, it's up to us!. The kitchen is the germiest room in the house-- teeming with billions of microorganisms on countertops, refrigerators and cutting boards. And the worse culprit: the kitchen sponge! A migraine is the most common type of headache that propels patients to seek care from their doctors. Roughly 30 million Americans suffer from migraine headaches, with women affected almost three times more often than men, according to statistics from the National Headache Foundation in Chicago. Today's blog incorporates an article by Jennifer Wider, MD of the
A migraine is the most common type of headache that propels patients to seek care from their doctors. Roughly 30 million Americans suffer from migraine headaches, with women affected almost three times more often than men, according to statistics from the National Headache Foundation in Chicago. Today's blog incorporates an article by Jennifer Wider, MD of the 
 Spending time on a bicycle seat, which has been linked to erectile dysfunction in men, may also be a hazard to a woman’s sexual health, a new study shows.
Spending time on a bicycle seat, which has been linked to erectile dysfunction in men, may also be a hazard to a woman’s sexual health, a new study shows.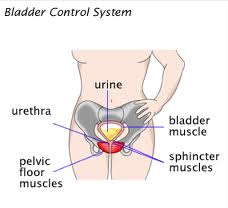 A type of exercise called pelvic floor muscle training is effective for treating adult women with urinary incontinence (the involuntary loss of urine) without risk of side effects, according to a new report from the U.S. Agency for Healthcare Research and Quality (AHRQ). The report also found that drug-based treatments can be effective, but the degree of benefit is low and side effects are common.
A type of exercise called pelvic floor muscle training is effective for treating adult women with urinary incontinence (the involuntary loss of urine) without risk of side effects, according to a new report from the U.S. Agency for Healthcare Research and Quality (AHRQ). The report also found that drug-based treatments can be effective, but the degree of benefit is low and side effects are common. Women take longer to give birth today than did women 50 years ago, according to an analysis of nearly 140,000 deliveries conducted by researchers at the National Institutes of Health.
Women take longer to give birth today than did women 50 years ago, according to an analysis of nearly 140,000 deliveries conducted by researchers at the National Institutes of Health. While we continue to fight for access to health care (pending the US Supreme Court decision on the Affordable Care Act) it's rewarding to see that work continues on economic and job issues. U.S. Senator Tom Harkin recently introduced the
While we continue to fight for access to health care (pending the US Supreme Court decision on the Affordable Care Act) it's rewarding to see that work continues on economic and job issues. U.S. Senator Tom Harkin recently introduced the  We tend to think of rural women's issues in the context of the developing world. But in America rural women also struggle. One of the big factors in rural poverty is the lack of access to decent health services. On March 30,2012, Worldview, a weekly talk show on WBEZ radio, a PBS affiliate, explored rural women’s health issues and needs in the U.S. with Sharon Green, the executive director of Northwestern University's
We tend to think of rural women's issues in the context of the developing world. But in America rural women also struggle. One of the big factors in rural poverty is the lack of access to decent health services. On March 30,2012, Worldview, a weekly talk show on WBEZ radio, a PBS affiliate, explored rural women’s health issues and needs in the U.S. with Sharon Green, the executive director of Northwestern University's